Hormonal birth control is commonly used to prevent pregnancy and to manage symptoms like acne, heavy bleeding, and painful cycles. While it can be helpful in the short term, it often masks underlying issues rather than resolving them, and those root causes may resurface once you stop taking it.
If you’re preparing to TTC, planning to stop birth control soon, or just want to understand how it affects your body, this guide will help you navigate the transition. We’ll cover how the pill works, how it may influence hormones, nutrient status, and other systems, and what you can do to support fertility after stopping.
What is birth control?
Birth control refers to a wide range of medications, devices, or procedures used to prevent pregnancy. They may also be used for other reasons, such as painful menstrual symptoms.
Oral birth control, aka “the pill,” is a common form used to prevent pregnancy or treat symptoms, and is commonly prescribed by health care providers.
Most oral contraceptives are made with combinations of synthetic (man-made) estrogen and progestin, a synthetic form of the hormone progesterone. These hormones enter the brain and act as endocrine disruptors, interfering with the signaling pathways necessary for ovulation.
In particular, they prevent the hypothalamus from signaling to the pituitary gland (which regulates your hormones) to secrete the hormones that cause an egg to be released. Without ovulation, pregnancy cannot occur. In the unlikely event that ovulation occurs and an egg is fertilized, the synthetic progestin thins the uterine lining, increasing the likelihood that the egg will be shed.
Many birth control pills include a week of placebo pills that induce monthly breakthrough or withdrawal bleeding, but this is not a true period (3)! This looks like a period, but it is not a true menstrual period because it doesn’t follow ovulation. It’s a bleed caused by the sudden drop in synthetic hormones.
For this note, the primary form of birth control we will be focusing on will be oral hormonal birth control, its associated side effects, and what you can do to replenish your body’s nutrient stores if you have been on it for any period of time!
Why can birth control be problematic?
There are valid reasons to use birth control, whether for contraception, acne, or painful periods. This guide isn’t a recommendation for or against birth control; it’s intended to provide context on physiological effects and how to support your body during transitions.
Many people start birth control to manage symptoms, believing it fixes the root cause. In reality, it often suppresses symptoms without resolving the imbalance, which is why issues like heavy bleeding, acne, or irregular cycles may return (or appear in new ways) after stopping. The pill doesn’t create new problems—it can simply mask what’s already happening.
It’s also important to remember: symptoms like debilitating periods, acne, or extremely heavy bleeding may be common, but they’re not normal. These symptoms have root causes that deserve to be addressed beyond a temporary hormonal override.
Where to start:
Increase nutrient-dense whole-food meals, especially quality proteins, seafood, leafy greens, and mineral-rich foods—to support hormone production and detox pathways. Pair this with a functional provider who can help you evaluate potential contributors, such as thyroid issues, gut health, and blood sugar regulation.
We’ll walk through each of these in more detail throughout this guide, so you know exactly how to support your body as you transition off birth control.
How does birth control affect different systems of the body?
Hormonal birth control works by overriding natural hormone rhythms, so it makes sense that it can influence more than just your reproductive system (4, 5).
Hormonal birth control pills provide synthetic hormones, which can lead to effects in all systems of the body:
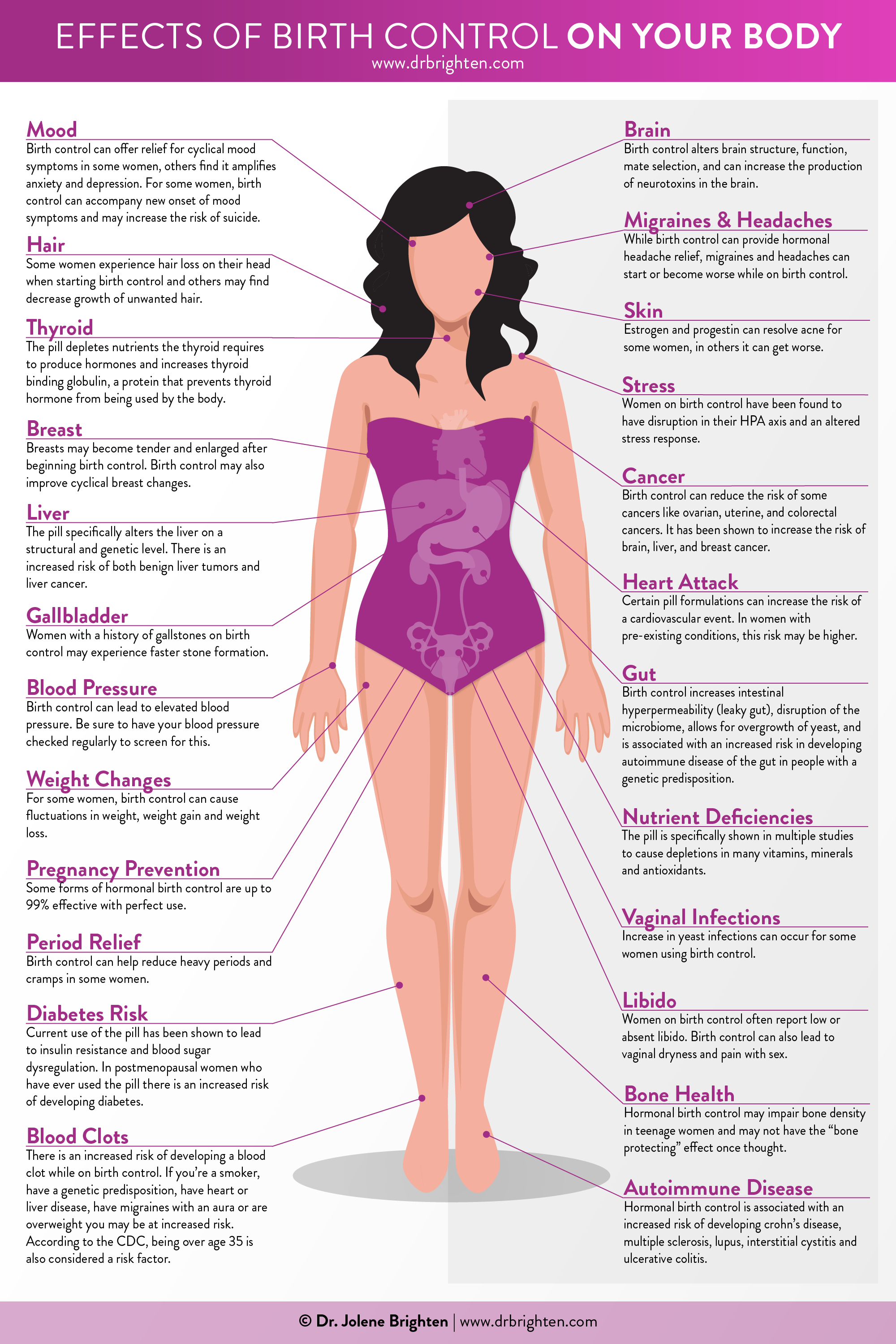
Hormone Signaling
Hormonal birth control suppresses communication between the brain and ovaries (the hypothalamus–pituitary–ovarian axis), preventing the natural rise and fall of hormones needed for ovulation. After stopping, your brain and ovaries often need some time to “reconnect” and resume regular, ovulatory cycles.
Nutrient Status
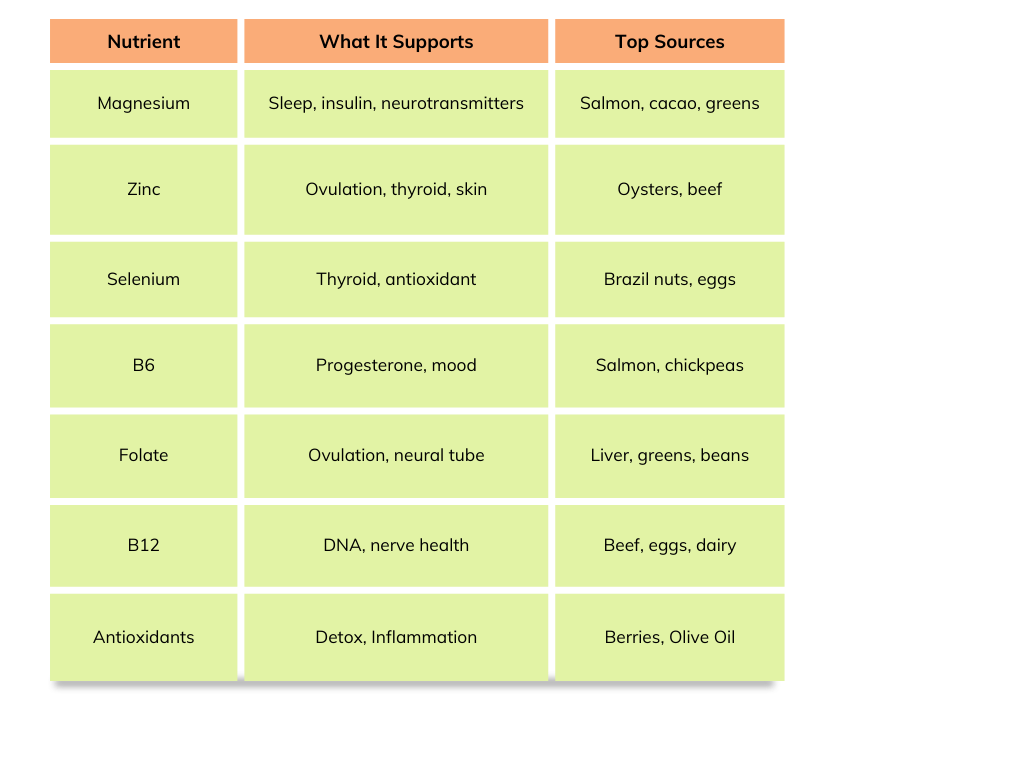
Some research shows that hormonal contraceptives may reduce nutrient levels or increase the body’s need for nutrients such as folate, B6, B12, magnesium, zinc, selenium, and antioxidant vitamins (4, 6, 7, 8). These nutrients are essential for ovulation, egg quality, thyroid function, mood, and detoxification, which is why replenishing them after stopping birth control can be highly supportive.
Thyroid Function
Estrogen-containing birth control increases thyroid-binding proteins, which changes how thyroid hormones circulate (9). This doesn’t usually cause thyroid disease, but it can affect lab results, and people with underlying thyroid tendencies may feel shifts. Checking thyroid labs after stopping birth control can be helpful if you notice fatigue, hair loss, or temperature intolerance.
Metabolism and Blood Sugar
Some hormonal birth control methods may influence insulin sensitivity or lipid levels in certain individuals (5, 10). Even if you didn’t feel these effects, stabilizing blood sugar through balanced meals and movement is an integral part of supporting hormone health going forward.
Liver and Estrogen Detoxification
Your liver metabolizes synthetic hormones. Your liver needs nutrients such as choline, B vitamins, and antioxidants to complete the detoxification process (11). Supporting liver health through whole foods, fiber, cruciferous vegetables, and healthy digestion becomes essential during and after stopping birth control.
Gut Health
Some studies suggest hormonal birth control may influence gut bacteria and intestinal permeability in certain people (12). Because gut health affects nutrient absorption, inflammation, and estrogen metabolism, nourishing your digestive system can help support hormone balance during the transition off birth control.
Mood and Brain
Responses to hormonal birth control vary widely. Some feel their mood improves, some notice anxiety, lower libido, brain fog, or emotional changes (13, 14). These effects may be due to shifts in neurotransmitter levels, altered brain hormone receptors, or nutrient depletion. If you noticed mood changes on or off birth control, your experience is valid and worth bringing up with a provider.
Can birth control affect fertility?
The good news is that hormonal birth control does not cause permanent infertility in people who were otherwise fertile (15). But because it suppresses natural hormone signaling, fertility may take time to return as your body re-establishes regular ovulation (16).
If you had underlying conditions before starting birth control, such as PCOS, thyroid dysfunction, or irregular cycles, those patterns may resurface once synthetic hormones are removed. This can extend the timeline for restoring optimal fertility, not because birth control caused new problems, but because it temporarily masked existing ones.
This does not mean that getting pregnant after birth control is impossible. Still, it does mean that if you have been on birth control before trying to conceive, it’s most realistic to recognize it could take some time to get back to an optimal fertile state (this depends on your unique physiology, health, and how long you were on birth control).
Most people resume ovulation within a few months after discontinuing hormonal birth control (17, 18). IUDs and implants may allow faster return to fertility once removed, while the Depo shot may take the longest (sometimes 6–12 months).
If cycles don’t return or remain irregular after several months, consider evaluating thyroid function, blood sugar balance, and nutrient status with a knowledgeable provider.
What should I expect when stopping BC?
Transitioning off birth control looks different for everyone. Your experience will depend on your health before starting, the type of birth control you used, and how long you were on it. Some people transition very smoothly, while others experience symptoms, such as:
- Irregular cycles at first
- Temporary anovulatory cycles
- Acne flares
- Mood shifts
- Heavier or lighter bleeding
- Changes in cervical mucus
- Cramps or PMS symptoms that were previously masked
All of these changes reflect your body transitioning out of a hormonally suppressed state and back into its natural cycle. If you don’t get a bleed within three months or if symptoms are extreme, talk with a healthcare provider.
What labs should I consider testing after stopping BC?
If cycles are slow to return or you want a full picture of your hormone health after stopping birth control, lab testing can offer important insights and identify areas that need support. A comprehensive lab panel to consider discussing with your provider may include:
- Estradiol, progesterone, LH, FSH, prolactin
- TSH, free T3, free T4, thyroid antibodies
- Comprehensive iron panel
- Vitamin D, B12
- Hemoglobin A1c, fasting insulin, and glucose
- Lipid panel
These labs can help determine whether your thyroid, blood sugar, or nutrient status is affecting ovulation.
Since hormonal birth control can influence mineral status, HTMA testing can be another helpful tool after stopping birth control. HTMA measures mineral levels and ratios in hair tissue, which reflect longer-term mineral patterns.
Because minerals are foundational for hormone production, thyroid conversion, blood sugar balance, and nervous system regulation, identifying imbalances through HTMA can help tailor a targeted nutrition plan to support fertility.
See if we have available HTMA spots under “nutrition services.”
What can I do to optimize fertility after coming off BC?
To support your body in resuming optimal fertility, focus on nourishment, replenishment, and consistent daily habits that support hormone health. Small daily habits can offer meaningful support in helping your body re-establish its natural hormonal rhythm and restore healthy ovulation.
Rebuild nutrient stores
Evidence suggests that oral contraceptives may lower levels or increase requirements of several key nutrients, especially those involved in methylation, neurotransmitter production, ovulation, and detoxification, including (20, 21, 22):
- Magnesium: supports insulin sensitivity, sleep, neurotransmitter regulation, and muscle relaxation. It’s one of the more common post-pill deficiencies (23, 24).
- Selenium: essential for thyroid hormone conversion and protecting follicles from oxidative stress.
- Zinc: supports ovulation, egg quality, thyroid health, skin health, and immune function. It’s also used heavily during detoxification.
- B6 (Pyridoxine): helps your body make serotonin, regulate mood, and convert tryptophan into melatonin to support sleep. It’s also crucial for healthy progesterone production and a strong luteal phase.
- B9 (Folate): consistently shown to be lower in those using oral contraceptives (4). Adequate folate is essential for ovulation and fetal neural tube development.
- B12 (Cobalamin): Birth control can reduce B12 levels (20), which impacts red blood cell formation, nervous system health, and DNA replication, which are critical for conception.
Optimize Minerals
Minerals play a foundational role in hormone signaling and reproductive function. Even small shifts in mineral status can influence mood, cycle length, cervical mucus, and progesterone production.
The minerals most affected by hormonal contraceptives appear to be zinc, magnesium, and selenium, as we addressed above (21). Other minerals that may be impacted and play an essential role in fertility include copper, iodine, and iron.
Incorporate mineral-rich foods daily, such as oysters, beef, eggs, leafy greens, nuts, seeds, and seaweed, and consider a simple mineral mocktail made with electrolytes and trace minerals to support hydration and mineral balance.
For a deeper look at mineral patterns, a Hair Tissue Mineral Analysis (HTMA) can be beneficial. HTMA evaluates long-term mineral status and provides insight into copper–zinc balance, adrenal patterns, thyroid-related mineral ratios, and potential deficiencies that influence cycles and fertility.
Support blood sugar balance
Balanced blood sugar is one of the most underestimated fertility tools. Stable blood sugar is essential for healthy ovulation. Even mild insulin resistance can suppress ovulation, shorten the luteal phase, worsen PMS, and increase inflammation (25, 26).
Hormonal birth control may influence insulin sensitivity in some people. Additionally, if you started birth control to help manage PCOS symptoms, it’s important to know that PCOS often has a layer of blood sugar dysregulation. Coming off birth control may reveal this pattern.
Practical steps:
- Build meals with protein, healthy fats, fiber, and lots of color.
- Avoid going long periods without eating to prevent crashes and cravings.
- Incorporate regular walking and strength training.
- Avoid “lonely carbs” (i.e., carbs without protein and/or fat)
Work to improve gut health.
A healthy gut supports optimal nutrient absorption and hormone metabolism. Some research suggests hormonal birth control may shift gut bacteria or intestinal permeability in susceptible individuals (27, 28). Supporting gut health helps your body eliminate hormones efficiently.
Practical steps:
- Aim for 25-35g+ of fiber daily
- Include fermented foods (yogurt, kefir, sauerkraut
- Eat a wide variety of colorful plants each week
- Consume added sugar in moderation
- Drink plenty of water
Support thyroid health and hormone production.
The thyroid and progesterone work closely to maintain regular cycles. T3 and T4 influence ovulation, luteal phase length, and progesterone levels (29).
If you experience fatigue, cold intolerance, or very short luteal phases, supporting your thyroid with selenium, zinc, and iodine-rich foods may help. Adequate calories, stress management, and B6 also support healthy progesterone production.
If you experience these symptoms, additional thyroid testing may be indicated. Learn more about thyroid testing here.
Support liver detox
Your liver helps clear hormones, both synthetic and natural. Healthy detoxification doesn’t depend on “quick cleanses,” rather it depends on nutrients, blood sugar stability, and healthy digestion.
Practical steps:
- Include cruciferous vegetables daily (broccoli, brussels sprouts, cabbage)
- Eating enough protein (aim for 20-30g per meal)
- Add choline-rich foods (eggs, salmon, liver in moderation)
- Stay hydrated
- Support regular bowel movements to prevent estrogen reabsorption
- Limit alcohol to reduce liver burden
Learn more about liver health here.
Fertility-friendly lifestyle habits
Gentle lifestyle strategies support healthy ovulation, including:
- Get adequate amounts of sleep
- Manage stress (breathing exercises, meditation, walking)
- Avoid over-exercising (especially if periods are delayed)
- Ensure adequate caloric intake for your activity level
- Simple cycle tracking, such as cervical mucus observations
What are alternatives to standard birth control?
If you are looking to avoid pregnancy during this time, know that hormonal birth control does not have to be your only option.
Fertility awareness-based methods include:
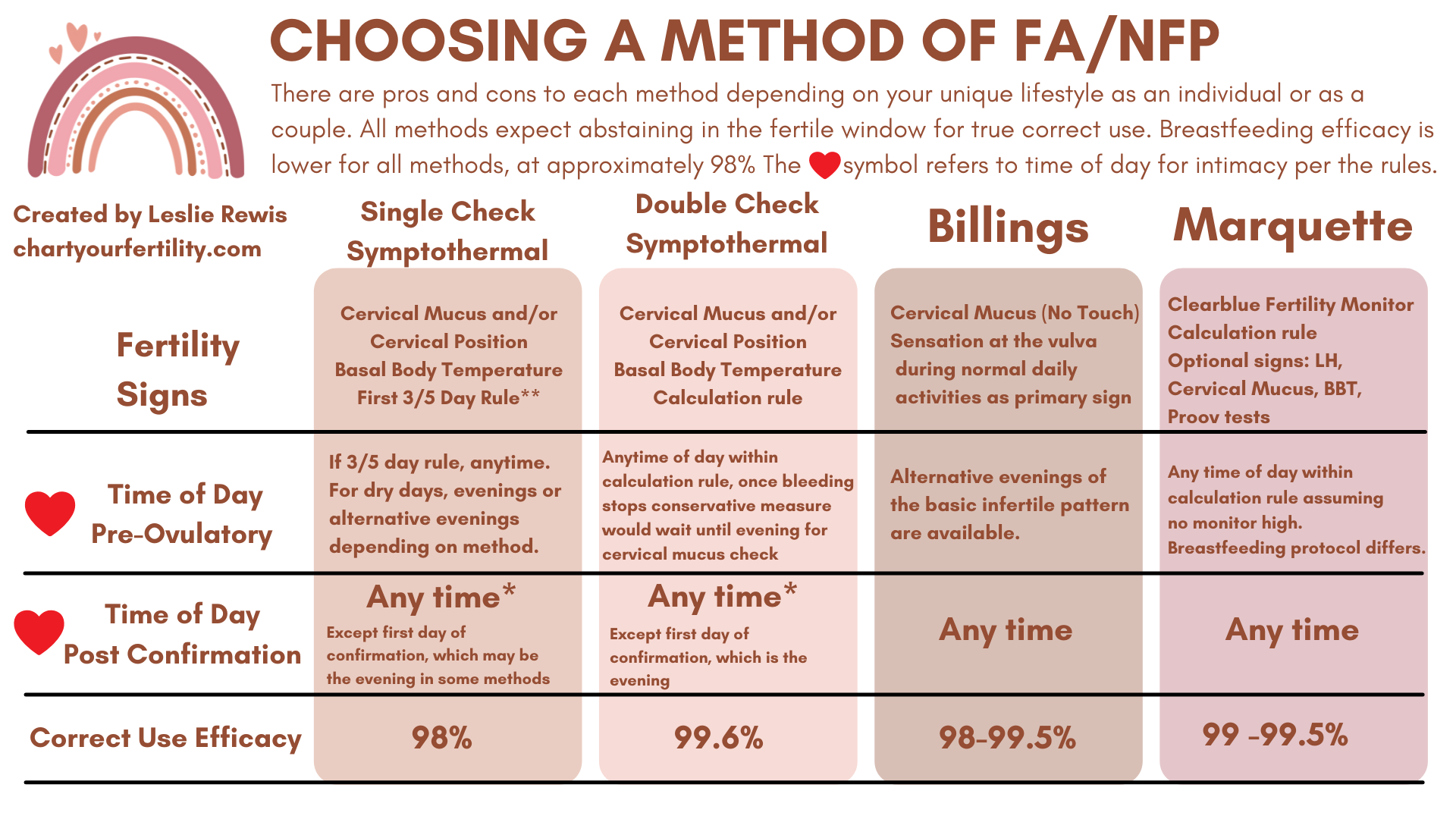
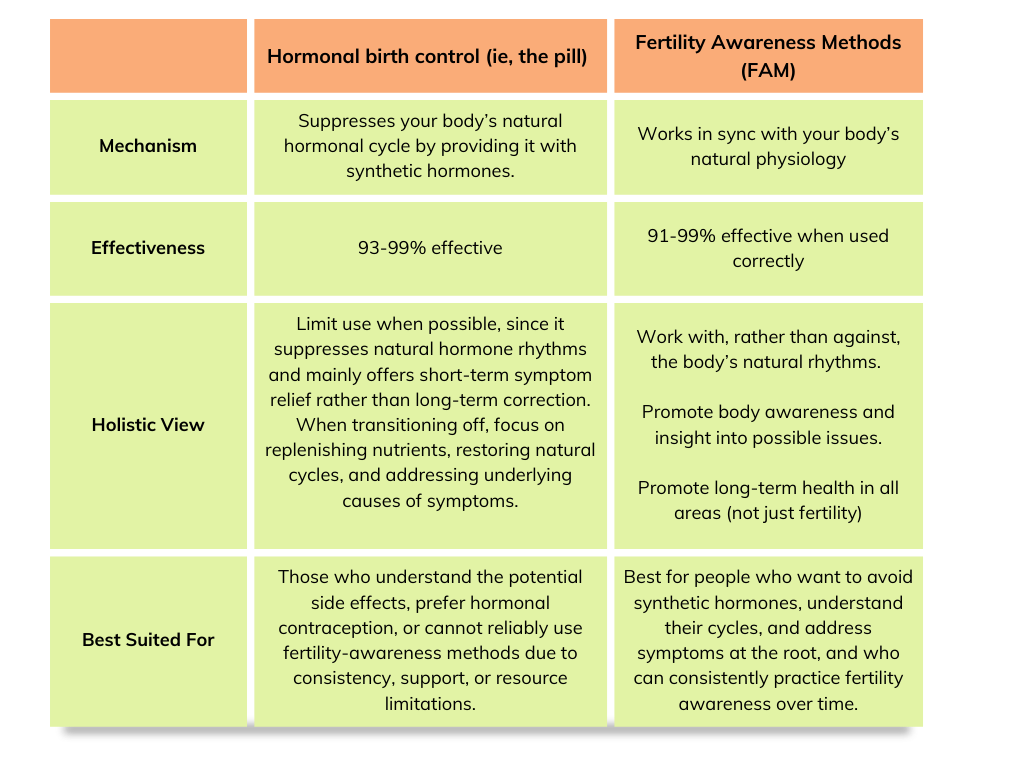
Fertility awareness-based methods teach you how to identify your fertile window using cervical mucus, temperature, or hormone tracking. When learned with an instructor and used correctly, these methods are incredibly accurate, at least as accurate as hormonal birth control (often, more so) (31). They also deepen your understanding of your cycle patterns.
Note that these take time and patience to learn! It’s ideal to start by working with a fertility educator who can help you interpret your body’s signs and patterns. Look for an instructor here.
If you are looking to gain more insight into your body and how it works through fertility awareness, here are some books and resources you can look into to learn more:
- The Fifth Vital Sign: Master your cycles and optimize your fertility
- Fertility Friday Blog– helping women understand their cycles and build body literacy by recognizing the menstrual cycle as a vital sign (podcast here as well)
- Taking Charge of Your Fertility
The Bottom Line
- Hormonal birth control prevents ovulation by suppressing communication between the brain and ovaries, which is why periods on the pill are withdrawal bleeds, not true periods.
- Hormonal birth control can be helpful for symptom management, but it often masks underlying issues (like PCOS, endometriosis, thyroid disorders, or blood sugar issues) rather than addressing their root causes.
- Your body can regain healthy fertility after birth control. Still, it’s not uncommon for ovulation and cycles to take some time to re-establish their natural rhythm, especially if underlying issues were previously masked.
- Nutrient depletion is well documented with oral contraceptive use, particularly of B vitamins, magnesium, zinc, selenium, and antioxidants. Replenishing these nutrients supports hormone balance and fertility.
- Stable blood sugar is an often underrated foundation for restoring ovulation, since even mild insulin resistance can delay ovulation, worsen PMS, shorten the luteal phase, and impact fertility.
- If you want non-hormonal birth control, fertility awareness-based methods can be effective options when used correctly and with plenty of practice.
Written by: Claire Gilmore, MSCN, CNS, LDN, and Jorden Edinger, MS, RDN, LDN
Reviewed by: Ryann Kipping, MPH, RDN, LDN
