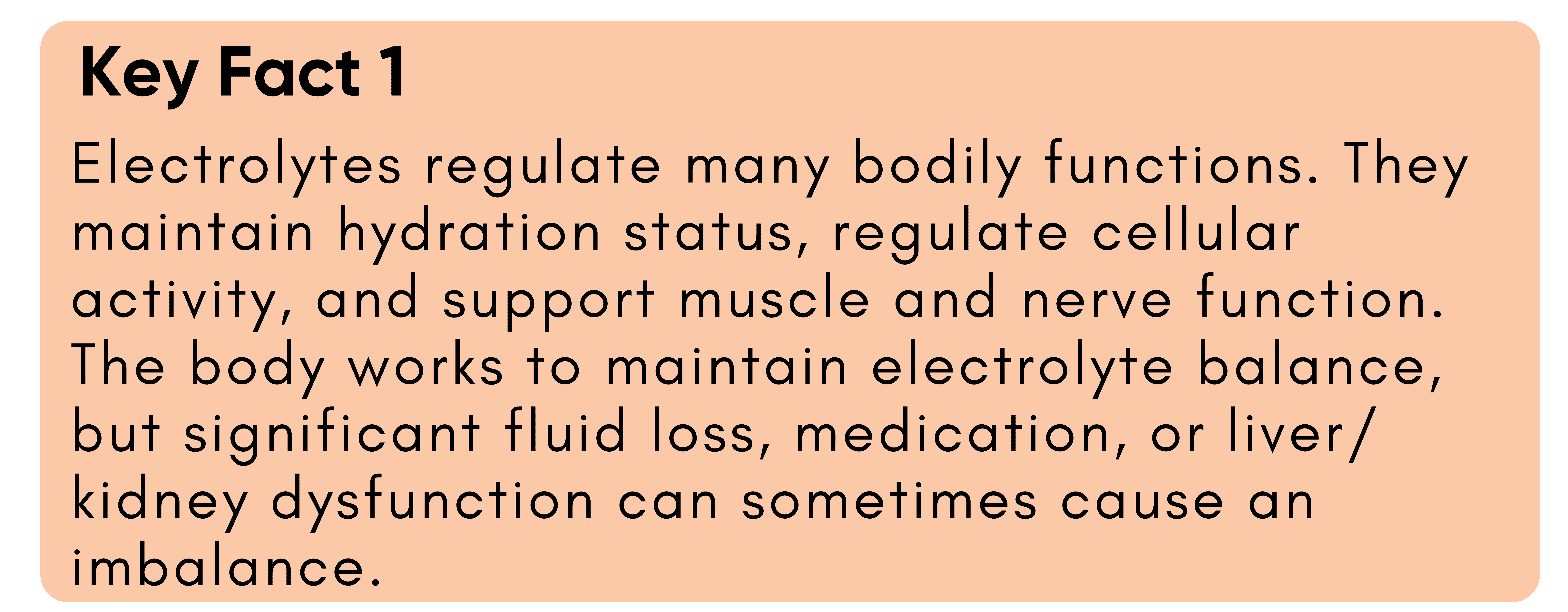
What are electrolytes?
Electrolytes are minerals with an electric charge that are essential to many functions in our body (1, 2).
Mostly, we hear about electrolytes and hydration, but they have many more jobs as well (1, 2), like:
- Balancing water in your body
- Balancing the pH in your body (acidity/alkalinity)
- Move nutrients into your cells, and waste out of them
- Regulate muscle contraction (like your biceps and your heart)
- Control nervous system function
3 major electrolytes are often discussed more than others. Can you guess them?
- Sodium
- Potassium
- Magnesium
There are others we don’t think about as much, but they are just as essential to our everyday functions:
- Calcium
- Chloride
- Phosphate
Why are electrolytes essential?
As mentioned above, we need them to survive. If the electrolyte levels in your body become too low or too high, this can wreak havoc on your nervous and muscular systems, your overall hydration status, blood pressure, and pH regulation (3).
If the amount of water in your body changes, your electrolytes will be considered “high” or “low.” Anytime you lose water, you lose electrolytes. This can occur through sweating, urine, diarrhea, vomiting, certain medications, and kidney or liver dysfunction (1, 2, 3).
That is why it is essential to keep hydrated and replace any water you lose throughout the day.
Some symptoms of electrolyte imbalance include (3):
- Muscle cramps, spasms, or weakness
- Irregular heartbeat
- Extreme thirst
- Fatigue
- Confusion
- Blood pressure change
- Swelling
- Seizure
Electrolytes & Fertility
Electrolyte balance should be monitored while trying to conceive (TTC). Sodium is associated with estrogen synthesis, and sodium, potassium, and calcium are involved in relaxing and contracting the uterus, all of which are critical aspects of reproduction (4).
Calcium and sodium are also involved in producing lipid hormones that develop follicles and regulate hormone secretion required for ovulation (4).
Lower sodium intake (<1500 mg daily) has been associated with lower progesterone levels, a hormone critical to the ovulatory process (5). Electrolyte disorders, including an insufficient calcium profile, have been shown to impact fertilization and embryonic development (4).
In most cases, your body can regulate electrolyte balance to perform the functions needed for conception. Still, it is helpful to remember their importance when TTC and make sure you are getting enough!
Electrolytes & Pregnancy
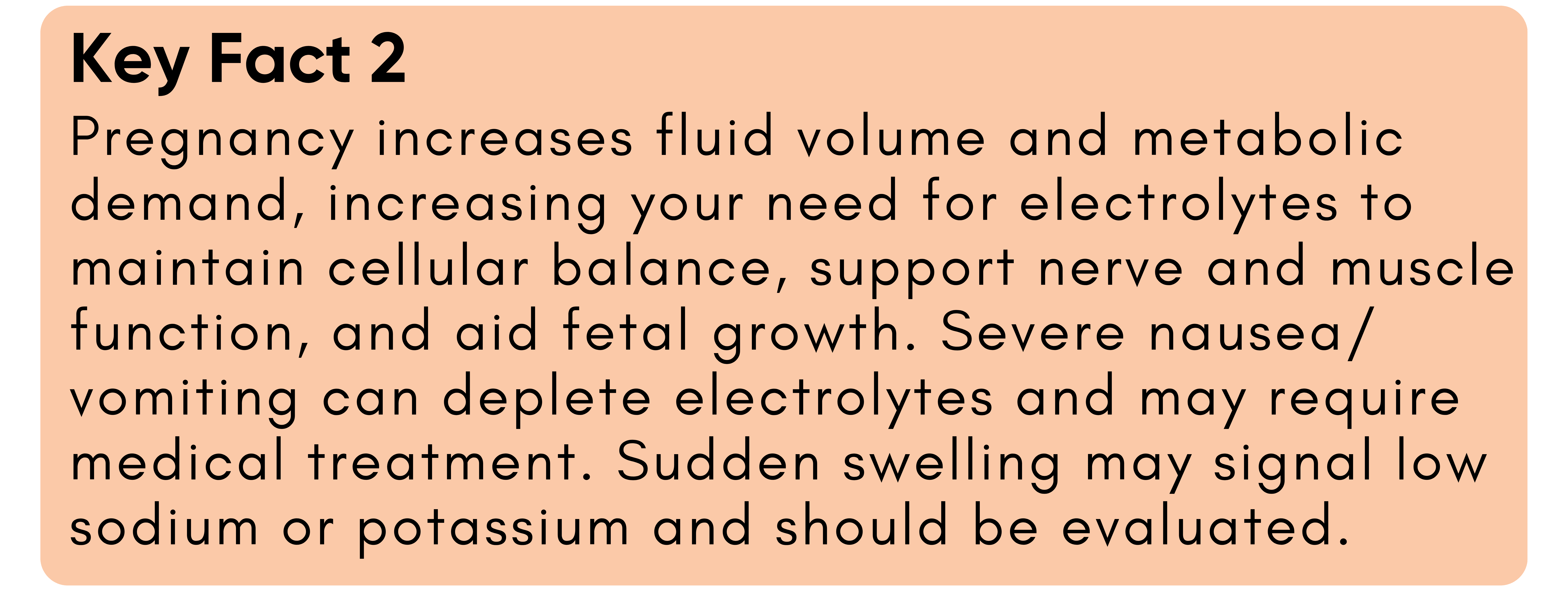
Pregnancy increases the demand on every system in your body, and with that comes greater fluid and electrolyte needs (6).
Electrolytes work hand in hand with fluids but play distinct roles. Fluids provide volume and transport, while electrolytes allow that fluid to move in and out of cells, maintain electrical signaling, regulate pH, and support normal muscle and nerve function. Drinking more water without adequate electrolytes won’t keep your body properly balanced (7).
Electrolyte needs rise during pregnancy to match increased fluid volume and the greater metabolic demands of both you and your baby. Getting enough nutrients from foods like fruits, vegetables, dairy, nuts, and mineral salts helps support healthy blood pressure, digestion, and fetal development.
What to Watch Out for in Pregnancy
Certain pregnancy conditions can lead to electrolyte imbalances, and it is vital to recognize the typical symptoms so they can be addressed appropriately. We will discuss some of the more prevalent imbalances so that you know what to do if you encounter them.
Hyperemesis gravidarum
People experiencing hyperemesis gravidarum (HG) — a severe form of nausea and vomiting that can cause dehydration, electrolyte imbalances, and weight loss (8) — often require more than dietary adjustments alone. Hospital-based care is usually necessary to manage symptoms and restore hydration through IV fluids and electrolyte replacement.
Alongside medical treatment, ongoing electrolyte and nutrient replenishment is key to recovery. If you have HG, talk with your healthcare provider about medication options (9).
Use one of the electrolyte replacement options listed in this guide daily.
Swelling
While swelling can be normal and due to various causes during pregnancy, it can also be another sign of electrolyte imbalances, such as insufficient sodium relative to total body water (hyponatremia) and/or inadequate potassium (10, 11).
If you experience rapid-onset swelling, it is always worthwhile to contact your medical provider to discuss possible causes and rule out more serious complications.
Electrolytes for Postpartum & Lactation
Delivering your baby and entering postpartum is a huge milestone—you have just run a marathon (both birth itself and the nine months leading up to birth).
Pregnancy can leave your body significantly depleted, and consuming additional electrolytes is one way to begin nourishing and restoring yourself postpartum. Mineral replenishment and adequate fluid intake are essential to supporting tissue repair after birth (12).
Electrolytes are also critical for baby if you are breastfeeding, as electrolyte concentrations in breastmilk directly affect your baby’s intake (13). Breastfeeding mothers are at risk of dehydration due to substantial water loss from lactation (approximately 700 mL daily at 8 weeks postpartum) (14).
Aim for about 16 cups of fluid daily, including at least one electrolyte-containing drink, and support your mineral needs by salting your food well and choosing calcium-, magnesium-, and potassium-rich foods.
How many electrolytes do I need at each stage?
Your electrolyte needs shift slightly throughout the perinatal journey because your fluid balance, blood volume, and hormone activity change. Let’s break it down.
While trying to conceive:
While trying to conceive, electrolyte needs should reflect the ranges recommended for healthy adult females. During this period, a key thing to remember is to avoid going low on sodium, as explained above, because this can affect progesterone levels.
- Sodium: Varies per individual; Up to 2300 mg/day (avoid going below 1500 mg – there is insufficient evidence to support low sodium recommendations, even for those with high blood pressure (15, 16))
- Potassium: 2300–2600 mg/day (17)
- Magnesium: 310–320 mg/day (18)
- Calcium: 1000 mg/day (19)
During Pregnancy:
As explained above, electrolyte needs increase slightly to maintain hydration during pregnancy.
- Sodium: Varies; we do not recommend tracking during pregnancy, as both you and baby need sufficient salt. Salt food to taste, and listen to your body’s cravings for salty foods!
- Potassium: 2600–4000 mg/day (17)
- Magnesium: 350–400 mg/day (18)
- Calcium: 1000 mg/day, more if underconsumed in adolescents (19)
Postpartum/ Lactation:
Breastfeeding places significant demands on your body, and your electrolyte needs are heightened to support you and your little one. Even if you are not breastfeeding, it is a good idea to consume ample electrolytes in the early postpartum period, as your body is in repair mode post-birth.
- Sodium: Again, this varies, and limiting sodium is not necessary. Salt food to taste, and eat salty foods if you are craving them.
- Potassium: 2500–2800 mg/day (17)
- Magnesium: 310–320 mg/day (18)
- Calcium: 1000 mg/day (19)
Where can I get electrolytes from?
Now that you’ve learned how essential electrolytes are at each stage, here is the good news: electrolytes are found in almost everything we eat and drink.
If you eat a varied diet with lots of colorful fruits, veggies, protein, and dairy sources, you get lots of electrolytes daily. Read to learn which foods and beverages are richest in key electrolytes.
Food
Yes, food has electrolytes! And, this is a great way to get them if you aren’t sweating a lot, vomiting, or having diarrhea.
Spinach, kale, avocado, broccoli, soybeans, tofu, almonds, strawberries, watermelon, oranges, bananas, tomatoes, milk, turkey, raisins, olives, canned soup, and many more all have multiple electrolytes.
If you want to get specific, the foods below are rich in the following electrolytes:
- Magnesium-rich foods: pumpkin seeds, chia seeds, almonds, spinach, cashews, dark chocolate
- Potassium-rich foods: dried apricots, lentils, prunes, acorn squash, potatoes, kidney beans, bananas, avocados, root veggies, spinach
- Calcium-rich foods: yogurt, kale, broccoli, canned sardines, salmon with bones, tofu, chia seeds, almonds
Drinks
Many fluids also contain electrolytes. Dairy milk, plant-based milks, fruit juice, coconut water, bone broth, and many smoothies are examples of beverages that naturally contain electrolytes.
Let’s break down which beverages are rich in key electrolytes:
- Magnesium-rich beverages: coconut water, watermelon juice, orange juice, celery juice
- Potassium-rich beverages: milk, coconut water, bone broth, watermelon juice, orange juice, lemon juice, celery juice, beet juice
- Calcium-rich beverages: milk, kefir, bone broth, soymilk, fortified almond milk, fortified orange juice, celery juice
Electrolyte Powders & Premade Drinks
Premade electrolyte beverages and powders contain many of the same ingredients, just in different amounts. It is essential to read the label to know exactly what you are getting.
Each brand varies in the amount of sugar, the type of sweetener, the amount of electrolytes, and the sources.
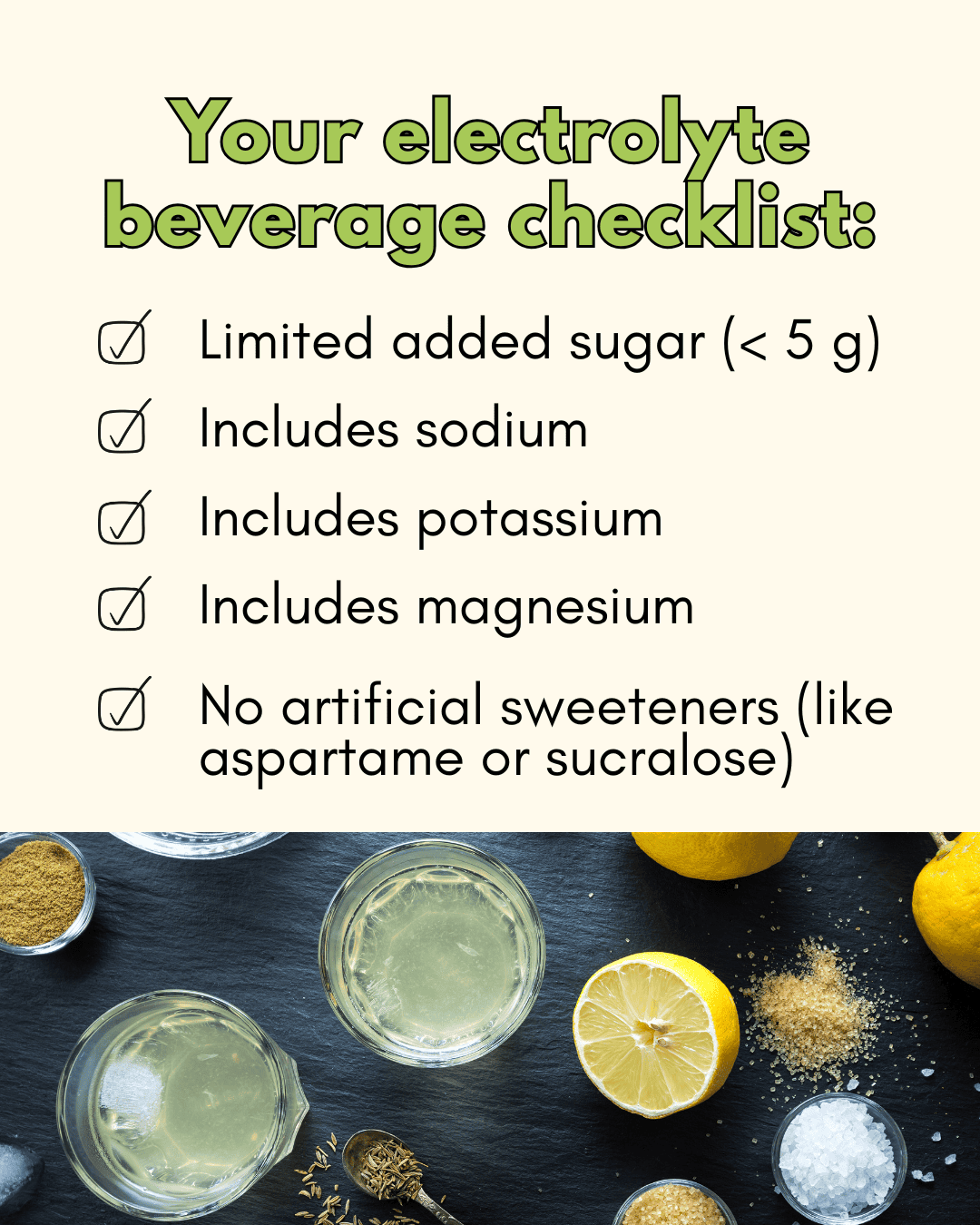
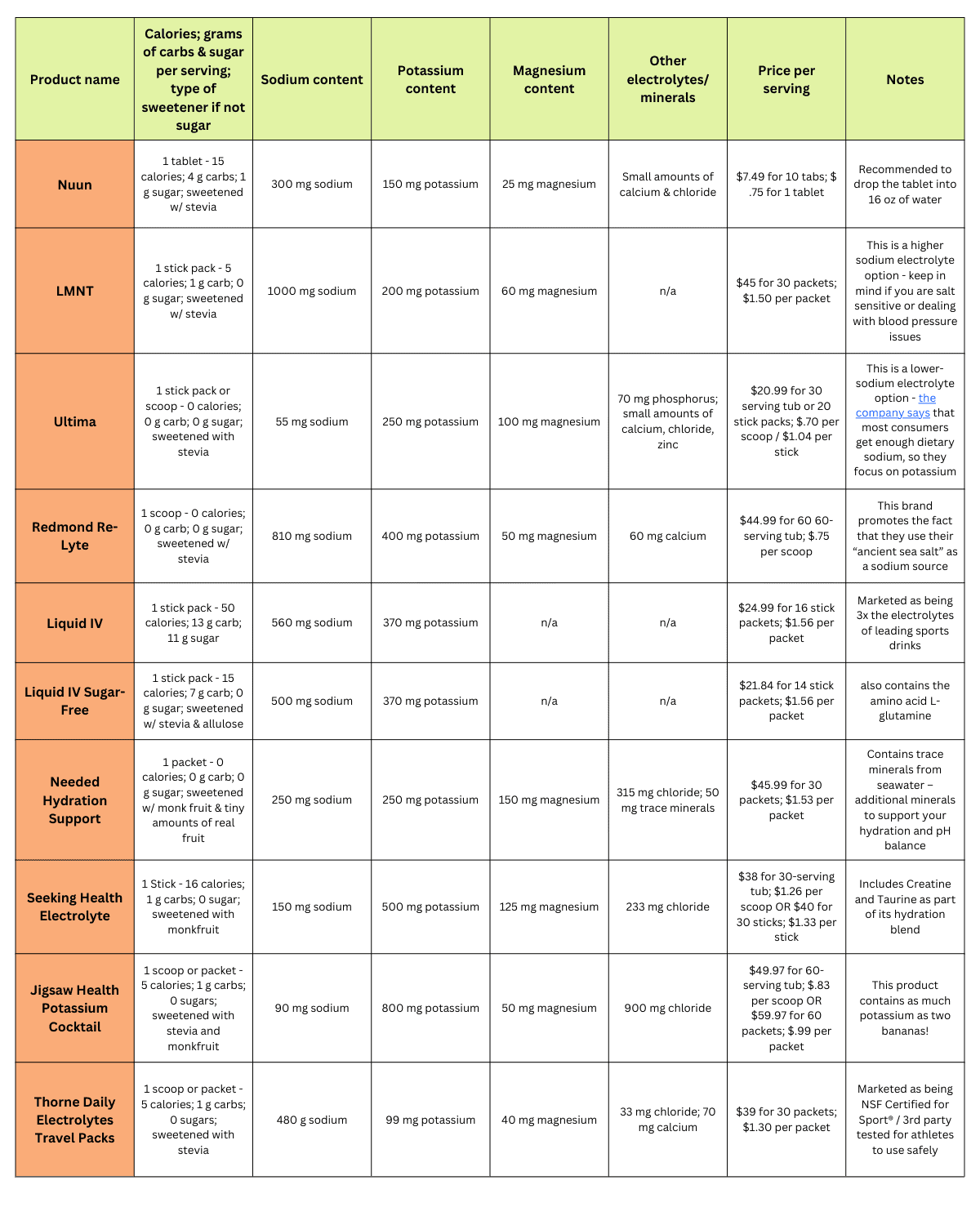
See Table 1 for ready-to-drink beverages and Table 2 for powdered options that you need to mix with water.
Table 1: Electrolyte Beverages (ready-to-drink):
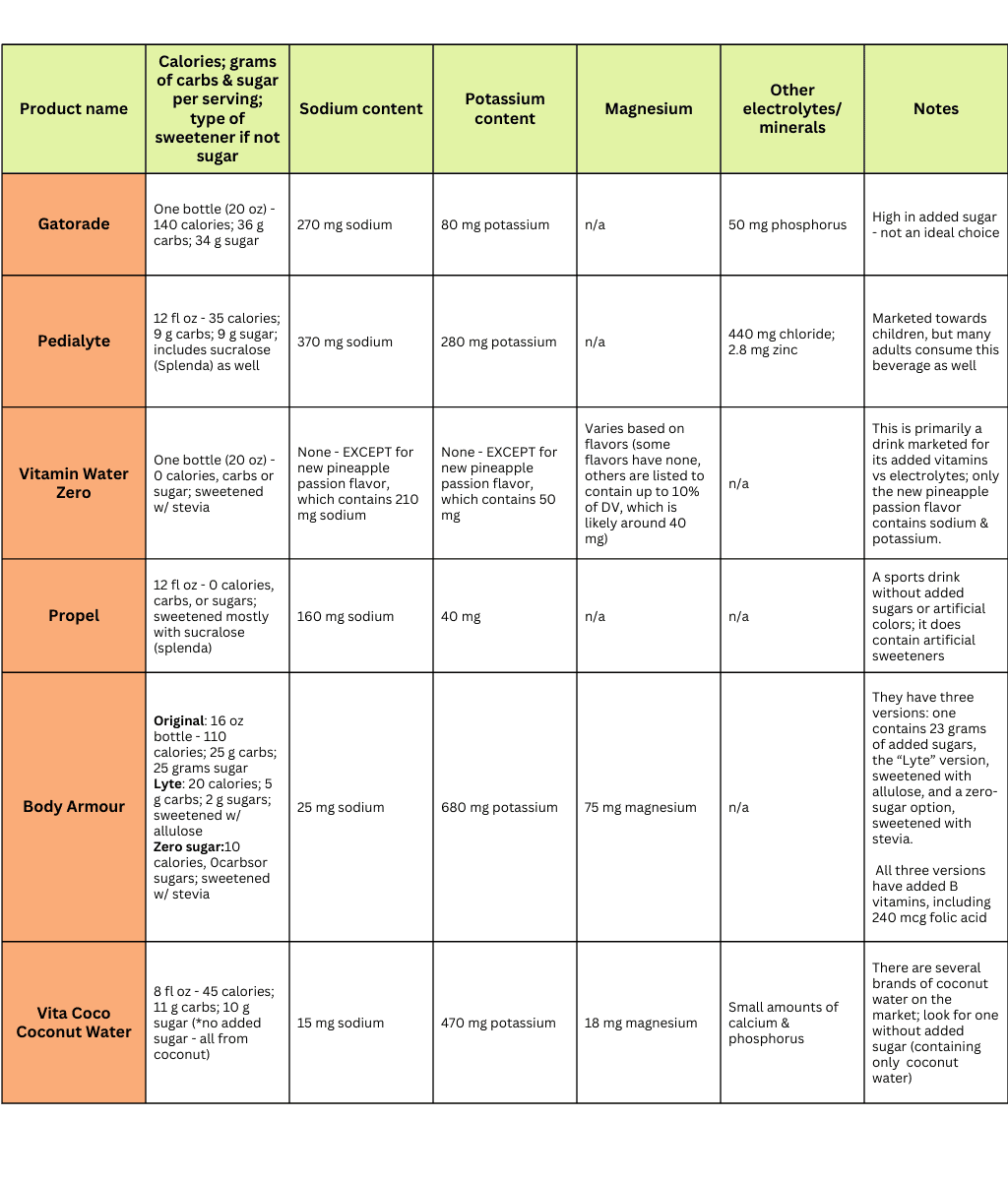 Table 2: Electrolyte powders (must be mixed with water):
Table 2: Electrolyte powders (must be mixed with water):
Top Electrolyte Powder Picks:
- Needed Hydration Support (code: TPNL)
- Seeking Health Electrolyte Sticks (Code: RyannK)
- Jigsaw Health Potassium Cocktail
- Thorne Daily Electrolytes Travel Packs
- Redmond Re-Lyte

How to make your own electrolyte beverage
It is also easy to make your own electrolyte-rich drink mix.
The basic formula is to combine a sodium source (like a pinch of sea salt) with a potassium and magnesium source from above, such as orange juice and/or coconut water. There are endless combinations to try, and you can get creative with the different minerals!
Check out our mineral mocktail guide for examples, including a fantastic lemonade and our favorite Mango Creamsicle mocktail.
To get you started, here is a super simple DIY recipe:
Electrolyte Balance Recipe
Ingredients:
- 1 lemon, juiced
- ½ cup apple juice or orange juice, 100% fruit juice
- ¼ tsp sea salt
- 1-liter coconut water, unsweetened
Directions:
- Wash the lemon. Juice the lemon in a separate bowl, then pour it directly into the decanter.
- Add the lemon juice, fruit juice, stevia, and sea salt to a medium-sized decanter.
- Lastly, add the coconut water and stir to combine.
Side effects and cautions
It’s hard to overdo electrolytes from food alone. Excess intake is more likely from multiple electrolyte drinks or powders—limit to no more than two per day unless your healthcare team advises otherwise.
Here are a few complications of electrolyte imbalance, for awareness:
Hypernatremia (high sodium)
Occurs when water loss exceeds sodium loss or when sodium intake is too high (8). Taking electrolyte powders without adequate water can contribute. Other causes require medical evaluation.
Hyperkalemia (high potassium)
Extremely rare from food; no upper limit exists for dietary potassium in healthy adults (17). People with impaired kidney function or on medications like ACE inhibitors should avoid large supplemental doses (17).
Hypermagnesemia (high magnesium)
Typically linked to very high intakes from magnesium-containing laxatives or antacids (18). While rare from a regular diet or supplements, a supplemental UL (tolerable upper limit) of 350 mg/day exists (18). This limit applies only to supplements. Consuming abundant magnesium from food sources is perfectly safe—you will not overdo it!
Calcium and phosphate excess are also uncommon and are usually associated with medications or underlying conditions (19, 20).
Mineral Ratios & Functional Testing
Electrolytes are a specific subset of minerals that carry an electric charge when dissolved in water. This charge allows them to conduct nerve impulses and regulate fluid balance. In other words, all electrolytes are minerals, but not all minerals are electrolytes.
Because electrolytes and minerals work together, their ratios matter as much as their individual amounts. Each mineral influences how the others are absorbed, stored, and utilized, and when one is out of balance, it can ripple through the entire system.
Example ratios:
- Sodium: Potassium—The Vitality Ratio tells us a lot about our stress response. It represents not only how our adrenals are functioning but also how our kidneys are functioning!
- Calcium: Magnesium—The Blood Sugar Ratio. Imbalances in this ratio can lead to high and low blood sugar!
- Calcium: Phosphorus—The Nervous System Ratio. This ratio tells us our “metabolic type,” such as slow or fast.
During pregnancy and postpartum, these ratios naturally shift in response to blood volume expansion, hormonal changes, and recovery demands. Tracking how you feel, energy, hydration, muscle function, and stress resilience can give early hints of imbalance, but functional testing offers clearer answers.
Functional Testing: HTMA
For a deeper look at your mineral and electrolyte status, the Hair Tissue Mineral Analysis (HTMA) provides a non-invasive way (cutting a small piece of your hair) to assess long-term mineral patterns. It can reveal chronic deficiencies, exposure to toxic elements, and the balance among key minerals such as sodium, potassium, calcium, and magnesium.
HTMA results can complement bloodwork and help personalize your electrolyte and mineral support across all perinatal stages.
Learn more about it here! Book your HTMA bundle with our team of dietitians under “nutrition services.”
The Bottom Line
- Electrolytes are charged minerals that keep your body functioning. They regulate hydration, pH, nerve and muscle activity, and nutrient transport. During the perinatal journey, your electrolyte needs shift as blood volume, hormone levels, and fluid balance change.
- Maintaining adequate sodium, potassium, calcium, and magnesium supports hormone production, ovulation, and uterine function while trying to conceive.
- During pregnancy, electrolyte and fluid requirements increase to support blood volume expansion, digestion, and fetal growth. Sodium, in particular, plays a vital role in blood pressure regulation and hydration. Salt restriction is outdated and unnecessary for most healthy pregnancies.
- In the postpartum and lactation phases, electrolytes help replenish losses from birth and breastmilk production, aiding recovery and sustaining milk supply.
- Electrolytes are found in many foods and beverages, such as dairy products, fruits, vegetables, coconut water, and bone broth. Regularly include a variety of electrolyte-rich foods in your diet.
- If you use an electrolyte supplement or beverage, choose one with limited added sugar, no artificial sweeteners, and sodium, potassium, and magnesium included. If you have the time, try making your own electrolyte beverage! You will likely save money and can customize the ingredients.
- Remember, electrolytes are minerals, and their ratios matter. Staying attuned to your symptoms and considering HTMA testing can provide deeper insight into your mineral balance.
Written by: Blair Strickland, Dietetic Intern, and Ryann Kipping, MPH, RDN, LDN