Why do some people get headaches during pregnancy?
Some people may be more prone to headaches during pregnancy than others, usually those who experience headaches or migraines frequently outside of pregnancy (1). Even outside of pregnancy, hormones play a big role in the development of migraines.
Headaches are usually more prevalent in the first and second trimesters. Most headaches during pregnancy are tension headaches, but could also be clusters or migraines. Some women who experience migraines outside of pregnancy notice a reduction in them during pregnancy– one study found up to 85% of people actually notice remission of migraines during pregnancy (but if you’re not part of this group that goes into remission during pregnancy, we cover migraines more below) (2).
Hormonal shifts, weight gain, and higher blood volume may all be contributors to headaches during pregnancy (1). Headaches in the later stages of pregnancy may be a sign of high blood pressure and should therefore be considered a red flag to mention to your doctor (3).
The good news is that there are many modifiable factors that you can do to help reduce your risk of developing headaches, their overall severity and frequency, and their management of them during pregnancy.
How can hydration levels impact headaches?
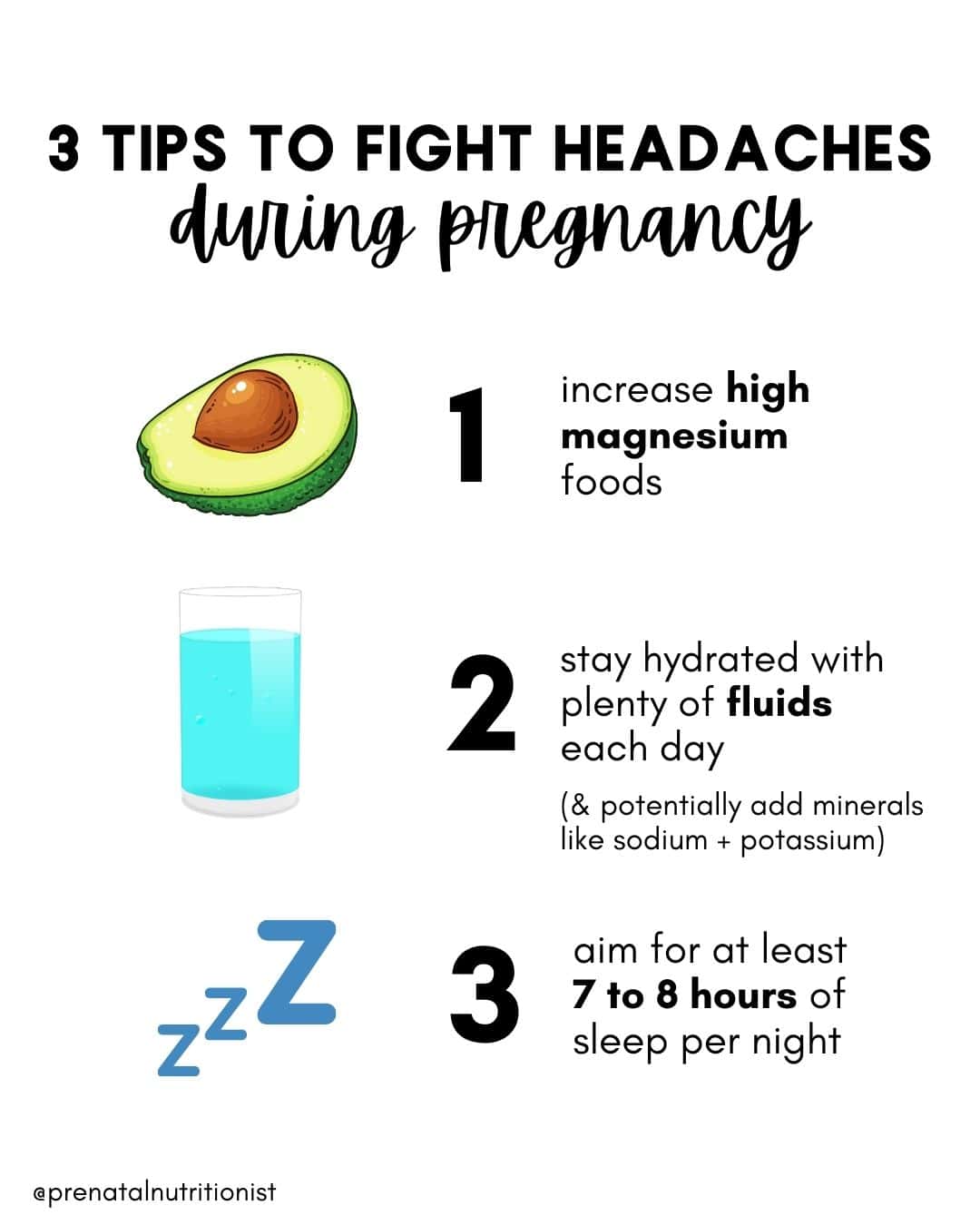
This might seem obvious, but sometimes we need constant reminders of how important water is, especially if you are prone to headaches. One hundred ounces of fluids per day is a good goal, which includes all fluids, not just water.
However, only drinking lots of plain water isn’t always enough to fully hydrate your cells, which means you could be drinking all the water in the world, but your cells aren’t actually absorbing it, so you continue to be dehydrated.
What is cell hydration, and why is it significant for overall hydration in the body? Let’s discuss it!
What is cellular hydration, and how can I boost it?
Feel like you’re always chugging water but never satisfied? Always thirsty and feeling like it goes right through you?
These are signs your cells aren’t actually absorbing the water you’re taking. You need to boost your cellular hydration by drinking water with minerals! Minerals, which also function as electrolytes, are vital to ensuring proper hydration on a cellular level because they help cells attract water (4).
Here are some ways you can boost your cellular hydration:
- Get minerals in both your food and drinks: Enhance your cellular hydration with sodium by simply adding a dash of unrefined salt to your water, and increase your intake of mineral-rich foods: fatty fish and dairy (calcium), leafy greens, nuts and seeds, and avocados (magnesium), cured and smoked meats, pickles, and olives (sodium), and unsweetened coconut water, dried fruit, potatoes, and greens (potassium)
- Eat fruits and vegetables high in water content with small amounts of other nutrients as well, such as watermelon, bell peppers, zucchini, oranges, and cucumbers.
- Monitor your individual symptoms of dehydration rather than count the number of glasses you drink daily. Besides headaches, these include fatigue, brain fog, irritability, muscle cramps, dark urine, and dry skin. (Read more about fluids here.)
 What nutrients can help with headaches?
What nutrients can help with headaches?
Magnesium
Magnesium has been found to reduce the incidence and severity of tension and cluster headaches, and most people aren’t getting enough of it (5).
Increase magnesium-containing foods and consider a magnesium supplement. Start with 100 mg of magnesium glycinate (if constipation isn’t an issue!) and gradually increase this dose if need be. Check out the magnesium note for supplement recommendations.
Foods rich in magnesium to increase your intake include nuts and seeds, cooked spinach, and beans.
Vitamin B12
Increase vitamin B12-containing foods and consider extra B12 supplementation. Some research suggests vitamin B12 needs during pregnancy are 3 times higher than we once thought. Make sure your prenatal contains methylcobalamin.
Foods highest in B12 to eat daily are beef liver, clams, salmon and tuna, beef, and dairy. (Remember: this vitamin is only found in animal foods, especially meats and fish, which is another reason why avoiding these during pregnancy is problematic. Read more here)
Omega-3’s
Many people aren’t getting enough omega-3s, which is important to note for both pregnancy in general and headache and migraine prevention. Some studies have found omega-3’s can be helpful in preventing these, likely due to their anti-inflammatory role, which we know is a common driving factor in migraine development (6, 7, 8, 9).
If you’re looking for ways to get in more omega-3s for both your and your baby’s brain, increase your intake of fatty fish (2-3 servings per week) or take high-quality fish oil (see recommendations here).
Probiotics
Not only are probiotics important for cultivating gut health for pregnancy in general (especially since you’ll pass your gut to your baby), but by supporting gut health which impacts brain health through the gut-brain axis, probiotics have also been found to be a helpful food for headache and migraine prevention!
One study (in children) found that using probiotic supplements seems to significantly affect the severity and frequency of migraine headaches compared to the placebo, and daily consumption of painkillers was significantly reduced in the probiotic group compared to the placebo group (10).
Many other studies have found similar results for probiotics reducing the frequency and intensity of attacks (11, 12, 13, 14).
Increasing your probiotic consumption through foods is the most ideal, especially if you’re consuming fermented foods like sauerkraut, kimchi, and miso at least 3 or more times weekly. Greek yogurt is another good source of probiotics.
Can sleep help with headaches?
Ensuring appropriate sleep is important, and lack of it may contribute to increased headaches (15). Aim for at least 7-8 hours per night and consult with a physical therapist if you need help determining appropriate sleep positions.
Getting enough quality sleep can be easier said than done during pregnancy-here are some tips to help you cultivate better sleep during this time:
- Create intentional wind-down time with a 20-minute (or more) bedtime routine. This routine can be a mix of the usual bedtime hygiene tasks (PJs, skincare, brushing teeth) as well as at least one more relaxing activity you enjoy to help you wind down: reading, journaling, an artistic activity, knitting/crocheting, prayer, or even a game with your spouse
- Sleep with your phone as far out of reach as possible (and resist the urge to check it in the middle of the night!)
- Make your sleep space conducive to good sleep: as dark and as cool as possible to reduce wakefulness and support better sleep quality (16)
- Drink a calming pregnancy-safe tea or one, especially for sleep support, such as a chamomile blend or Needed’s sleep + relaxation support.
Can exercise help with headaches?
Partaking in some form of exercise for 30 minutes 3 times per week has been shown to reduce the occurrence of headaches (keep in mind the national recommendation for exercise, in general, is 150 minutes per week, which means getting in 30 minutes at least 5 days per week) (17, 18).
Exercise doesn’t have to be intense to be effective, and ideally, it should always be a form of movement you enjoy! Walking, dance, a prenatal exercise class online or on an app…anything to support increased blood flow.
 Can eating certain foods trigger headaches and migraines?
Can eating certain foods trigger headaches and migraines?
While the exact causes of migraines are sometimes hard to pinpoint, for about 25% of people with migraines, certain foods can be identified as a contributing factor (19).
One possible reason could be that immune-mediated food sensitivities may be involved, as IgG antibodies can be a cause of inflammation (20). Identifying food triggers for some can be key for some in managing migraines; one study found that eliminating foods that led to these IgG reactions controlled migraines without the need for medication, while another found eliminating foods that led to IgG antibodies led to a significant reduction in the number of migraines or migraine-like headaches at four weeks (21, 22).
If you notice certain foods trigger headaches and migraines for you before pregnancy, these may be the same or different than they were before pregnancy.
Common triggers include (23):
- Caffeine (and caffeine-containing foods such as chocolate or teas)
- Artificial sweeteners
- Glutamic acid in MSG
- Foods high in tyramine: aged cheese, cured meats, pickled or fermented foods
- High-lactose dairy products
As you might notice, some of these foods are beneficial for pregnancy, so if you notice any correlation between a reduced tolerance of any of these and increased headache incidence (such as high lactose dairy and probiotic foods such as fermented foods), make sure you are replacing these with other food options that contain the same nutrients to ensure you are not missing these in your diet during this time.
If you suspect a food or food group could be triggering migraines, it’s recommended that you work with a licensed nutrition professional, as it’s not recommended that you self-diagnose food sensitivities and/or eliminate any whole foods (non-processed foods) during pregnancy.
Can I take medications to help me deal with headaches?
Consult with your physician before taking any medication during pregnancy. Usually, options during the first trimester are limited, but you may be able to take a pain reliever in the later stages of pregnancy. You can also check the Mother to Baby database.
In general, NSAIDs are discouraged, especially after 20 weeks of pregnancy, along with Ibuprofen and naproxen, but Tylenol is considered a safer medication to take during pregnancy (24).
You can also try alternative ways to deal with pain if you’re able, which are covered more at the end of this note.
What should I do if I’m dealing with migraines?
Migraines are complex issues, so if you’re dealing with this intensity level of headaches, it’s ideal to work with a functional practitioner who can help you investigate possible root causes of these. An estimated 10% of women deal with migraines during pregnancy (25).
Similar to regular headaches, migraines can be caused by rising estrogen levels during pregnancy, and though they can present for the first time during pregnancy without being tied to a specific condition (like preeclampsia), it’s always a good idea to mention them to your doctor (26).
Migraines can often be attributed to genetic, environmental, and lifestyle factors. While we don’t know exactly what causes migraines (especially as there are multiple possible contributors for each person), common triggers include:
- An overall pro-inflammatory and oxidative state (27)
- Insulin resistance (28)
- Inflammatory diseases (hint: nearly all diseases and conditions have inflammation as at least one partial root contributing factor (29)
- Mitochondrial dysfunction (30, 31)
- Stress, environmental allergens, and food allergies or sensitivities (32)
- Comorbid pain conditions
- Poor sleep
The good news is that aside from genetic factors, many factors can be modified by addressing these diet and lifestyle factors!
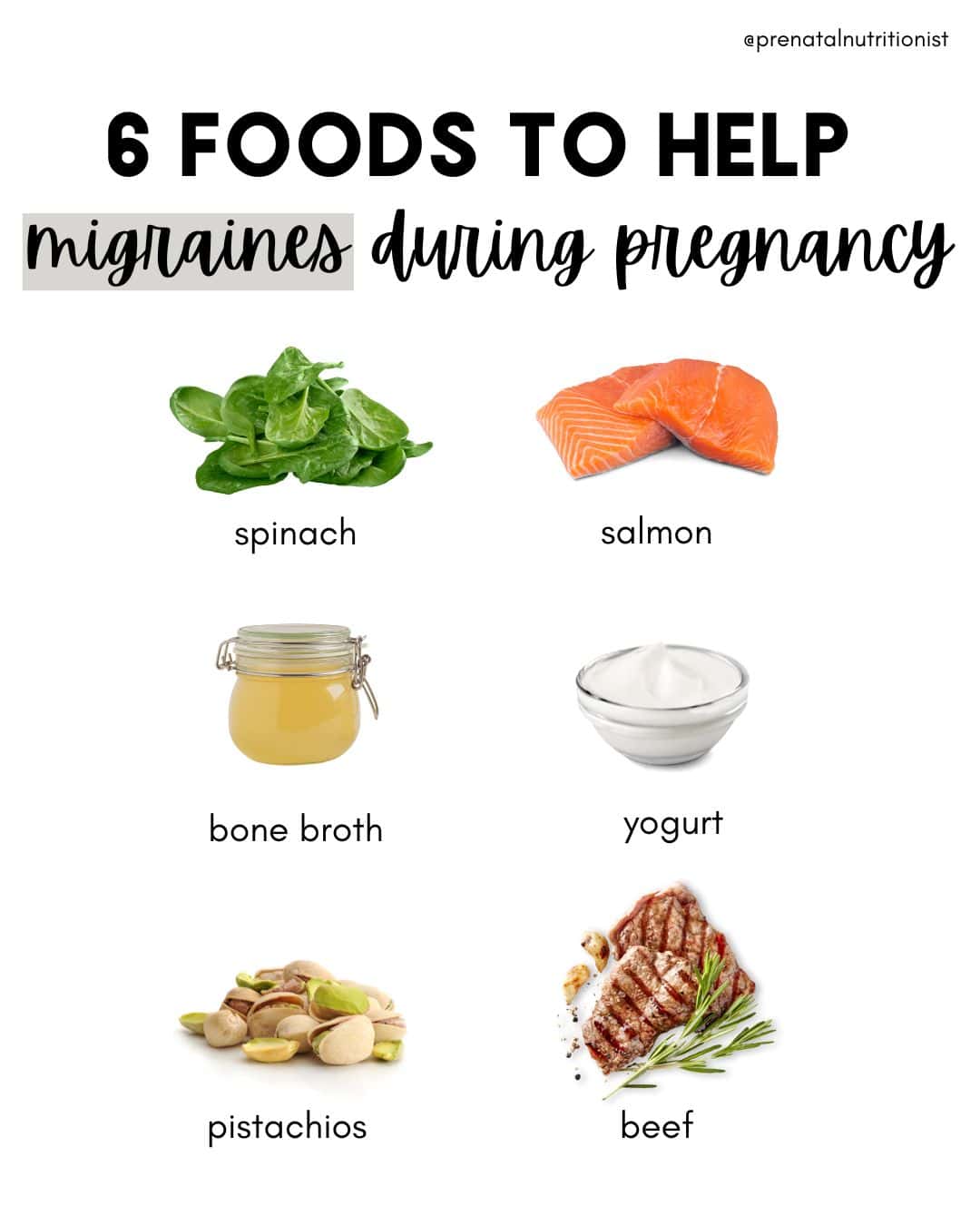
Nutrients and nutrition for migraines
Did you know there are specific nutrients that have been found to help support mitochondrial function and reduce the chances of recurring migraines?!
Nutrients that have been found to help prevent migraines include folate, riboflavin, coenzyme Q10, and magnesium (32).
It makes sense since folate can help with migraines because it is involved in DNA methylation, and research has found a folate-rich diet (one that is recommended anyway during pregnancy) can be an area to target migraine management and relief (33).
Studies have found that people with migraines often have increased levels of oxidative stress and pro-inflammatory cytokines, which riboflavin can help reduce, in addition to reducing migraine incidence overall (34).
Coenzyme Q10, aka CoQ10, has been found in studies to reduce migraine incidence, severity, and duration (35). Check out supplement recommendations in the CoQ10 note.
Magnesium is an important nutrient to focus on for headache and migraine prevention as well since studies have found at least 50% of people who get them are deficient in magnesium (36, 37). Being deficient in magnesium has been found to significantly contribute to the development of migraines (38).
So if you frequently get migraines, getting your magnesium levels checked and increasing your magnesium intake through food (and possibly a supplement if your levels are low) is a good idea!
A lower-carb diet for migraines
In addition to the nutrients above, a way of eating that has been specifically linked to helping manage many different neurological conditions, including migraines, is the ketogenic diet or a lower-carb diet (yes, it is safe during pregnancy– see our carbs note if you have concerns).
Because a low-carb diet supports cell processes in the brain and metabolism, along with mitochondria function, balanced serotonin levels, and neuroinflammation (39, 40).
Another reason a low to very low carbohydrate diet approach may be helpful for reducing migraines is that this is an effective way to manage blood sugar (41). Increasing evidence suggests that migraines may be the result of an impaired brain glucose metabolism, as well as dysfunctional mitochondria in the brain (42).
This could also be because peripheral insulin resistance has been thought to extend to the brain, leading to insulin resistance in the brain, and insulin resistance, in addition to metabolic syndrome, is more common in people with migraines (43, 44). (Just another reason why managing blood sugar matters for your overall health and helping you feel your best!)
If you are interested in implementing a distinctly low-carb diet during pregnancy, it’s highly recommended that you work with a licensed nutritionist or dietitian who can guide you in following one in a healthy way during pregnancy so you can ensure all your nutrient needs are met.
 What are other interventions that can help me manage headaches and migraines?
What are other interventions that can help me manage headaches and migraines?
Besides using a provider-approved pain reliever, here are some interventions you can try if you are looking for other alternatives, either instead of or in addition to pain-relieving meds:
- A headache cap
- Chiropractic care
- Massage therapy
- Acupuncture
- Addressing areas of stress and overall mental health
- Essential oils (do not ingest) like an aromatherapy stick for headaches and migraines (this one or this one)
- Stretching
- Extra rest
- Avoiding bright screens at night and wearing blue light glasses to limit eye strain (as this can trigger headaches)
- Drinking a soothing tea like this one (make sure you check the ingredients of any “headache tea” first, many include teas in blends that should be avoided during pregnancy)
When is a headache or migraine of concern during pregnancy?
Always mention headaches to your physician, especially if you have a family history of migraines, high blood pressure, seizures, or diabetes (45).
New or refractory headaches, hypertension, and abnormal neurological signs are important “red flags” to consider in particular (46). The Bottom Line
The Bottom Line
- A number of factors, like hormonal shifts, weight gain, and higher blood volume, could cause headaches during pregnancy.
- Aim for 100 ounces of total fluids per day with at least one glass per day with added salt or other sugar-free minerals to support cellular hydration.
- Eat foods high in magnesium, vitamin B12, omega 3s, and probiotics.
- Ensure you’re getting adequate sleep and physical activity every day, at least 7 hours of sleep each night, and 30 minutes of movement most days.
- If you’re dealing with migraines, make sure you’re getting enough riboflavin, coenzyme Q10, folate, and magnesium. Consider an additional magnesium or CoQ10 supplement.
- Consider lowering your carb intake. A low-carb diet has been found to be helpful for minimizing migraines, as well as addressing possible root factors, including inflammation, insulin resistance, mitochondrial dysfunction, stress, environmental allergens, food allergies or sensitivities, comorbid pain conditions, and poor sleep. Working with a functional practitioner to address these root causes is ideal.
- Review approved medication and/or other remedies to help with pain management, such as aromatherapy, chiropractic care, a headache cap, and drinking pregnancy-safe tea with your provider.
Written by: Ryann Kipping, MPH, RDN, LDN, and Claire Gilmore, MSCN, CNS, LDN