Author: Ryann Kipping, MPH, RDN, LDN
Fennel
Vitamin C

What is vitamin C?
Vitamin C is a water-soluble vitamin that must be consumed from our diet since the body can’t make or store it (1).
It’s an antioxidant that is often referred to as ascorbic acid. It’s essential for immune function, collagen synthesis, skin health, bone health, and blood vessel function/blood pressure.
What is vitamin C’s role in the body?
Vitamin C plays several key roles in our bodies, including (2, 3):
- Promotes collagen synthesis: Vitamin C works with enzymes to create amino acids unique to collagen structure– without vitamin C, we don’t have collagen!
- Assists wound healing
- Enhances iron absorption from plant-based foods
- Acts as an antioxidant against oxidative stress and cell damage
- Supports the immune system: Stimulates white blood cell protection, antibodies, and neutrophils, which are involved in the early immune response
- Helps repair and strengthen bones (including teeth) and cartilage
- Involved in the creation of neurotransmitters
- Helps us use copper in the body, and works with copper to signal to the brain to make thyroid hormone
- Involved in the physiology of the nervous system, supports the nervous system, and the stress response.
Is vitamin C important for fertility?
Vitamin C is a significant nutrient for both male and female fertility!
For females, vitamin C is involved in (4, 5, 6):
- Progesterone production by increasing the sensitivity of progesterone receptors
- Supporting egg quality by protecting against oxidative stress and cell damage
- Increasing endometrial thickness to support implantation
For males, vitamin C is involved in (7, 8):
- Protecting sperm from DNA damage from free radicals (oxidative stress)
- Improving sperm quality and motility
- Possibly increasing sperm count
Animal studies have found that a diet low in vitamin C induces a state of subfertility, reduces overall fecundity, and adversely impacts both pregnancy outcomes and growth in the offspring (F). These findings have been thought to apply to humans as well.
Is vitamin C important for pregnancy?
Due to inadequate intake, it is typically harder to enjoy fruits and veggies, and physiological changes during pregnancy decrease vitamin C levels, so trying your best to consume it regularly is essential.
Vitamin C is important for maintaining your immune system and preventing illness during pregnancy (9, 10).
Vitamin C and Birth Weight + Length
Several studies from South Korea have linked both vitamin C and vitamin E (both antioxidants) to positive birth weight and length outcomes (1, 2). They specifically mention that serum levels of vitamin C in the second trimester of pregnancy were predictive of birth weight and length.
It’s clear that the more fruits and vegetables you eat during pregnancy (for both these nutrients and more), the better!
Lower risk of pregnancy-associated conditions and complications
In a study with pregnant women who had type 1 diabetes, low vitamin C levels were found to be more problematic (11).
The researchers showed that inadequate vitamin C levels within 4 weeks of delivery were associated with a greater risk of pregnancy complications such as prematurity, pregnancy-induced hypertension, preeclampsia, fetal malformations, placental abruption, and stillbirth (12).
Again, these results were found in pregnant women with type 1 diabetes, and the number of participants was relatively small. Still, increasing vitamin C intake in the later stages of pregnancy is a good idea.
Supports iron absorption
Vitamin C also helps our bodies absorb iron better (13). This partnership cannot be understated during pregnancy.
Calcium can interfere with iron absorption (14), but studies have shown that in humans, this inhibition only lasts for a short while and typically doesn’t interfere substantially over a lifetime.
To boost iron absorption—especially from plant-based sources—pair high-iron foods with fruits and vegetables rich in vitamin C. Avoid eating high-calcium foods simultaneously, since calcium can interfere with iron absorption. This tip is most important if you’re a vegetarian or have low iron or anemia. If you regularly eat animal products and don’t have iron concerns, it’s less of a priority, but still worth noting.
See some high iron + vitamin C combos below.
Is vitamin C important for postpartum and breastfeeding?
Vitamin C is important for postpartum recovery and the health of the baby if you are breastfeeding (15, 16).
It’s a nutrient best known for supporting immune health, which is certainly important after giving birth. It is also needed for wound healing and collagen synthesis (13). These roles are essential for postpartum recovery and healing, especially if you’ve had a cesarean section or perineal tear during delivery.
Additionally, when working to replenish iron stores during postpartum, vitamin C helps enhance iron absorption. And since vitamin C modulates the response, it’s also critical for supporting your mental wellbeing during this vulnerable time (17).
Vitamin C is also present in breast milk to meet the baby’s needs (18). Some research suggests a maternal diet rich in vitamin C foods could increase the antioxidants in breast milk and reduce the risk of the infant developing some allergic conditions, such as asthma or eczema (19, 20).
How much vitamin C do I need?
You will likely meet vitamin C needs through food and a quality prenatal vitamin. However, a supplement could be indicated if you know you have a low vitamin C intake or a deficiency (21).
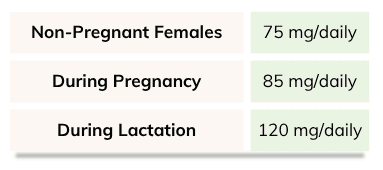
The following intake amounts are recommended:
Where do we find it?
Many fruits and veggies are good sources of vitamin C. Include a variety of the following regularly in your diet to meet your vitamin C needs before, during, and after pregnancy (22):
- Bell Peppers
- Kiwis
- Broccoli
- Strawberries
- Brussel sprouts
- Cantaloupe
- Cabbage
- Cauliflower
- Potatoes
- Spinach
Is it possible to be deficient in vitamin C?
Yes, it is possible to be deficient in vitamin C. However, it is more common in males than in females, who have about a 12 percent chance (the highest statistical chance in one’s lifetime) from ages 25-44 of becoming deficient (23).
Those at the highest risk of becoming deficient include those with medical conditions such as Crohn’s or celiac, which interfere with vitamin C absorption, and those with a diet low in fruits and veggies.
Should I supplement with vitamin C?
Vitamin C is likely in your prenatal vitamin and most generic multivitamins or “immune-boosting” supplements.
The most common form of supplemental vitamin C is ascorbic acid, which doesn’t contain tyrosinase or copper, which means it can’t provide you with all the benefits that vitamin C containing all its components can.
Ascorbic acid is a man-made, commercial form of synthetic processed vitamin C, designed to mimic natural vitamin C.
However, naturally occurring vitamin C contains ascorbic acid and other compounds and minerals, which are missing from the synthetic creation of ascorbic acid.
High doses of vitamin C, such as ascorbic acid, can also interfere with copper absorption and metabolism, decreasing copper status. While moderate intakes of ascorbic acid generally don’t cause significant problems (especially if they’re within a prenatal that also contains copper), high levels taken in isolation (such as those in immune-boosting supplements) can interfere with the body’s ability to absorb and utilize copper and can also deplete vitamin B12 (24, 25).
The most ideal way to supplement with vitamin C is in its whole food form, such as acerola and camu-camu. You can buy these in various forms (powders, capsules) and add them to a mineral mocktail, smoothie, or other beverage of choice.
Here are some recommended brands:
- Perfect Supplements pure acerola cherry powder
- Navitas organic camu powder
- Smidge Kakadu Plum Extract capsules (higher in vitamin C than any other food!)
- Camu Supreme Capsules
We recommend Needed’s Immune Support if you want a well-rounded, pregnancy-safe immune-boosting product. It does not contain vitamin C, so you could combine it with a vitamin C option from above. This product tastes great in water; add it to plain yogurt or a smoothie.
Other vitamin C-containing products and supplements
Vitamin C is also found in many different commercially available beverages.
One popular one is Emergen-C. One packet of this fizzy drink packs a massive 1000 mg punch of vitamin C (as ascorbic acid)! It also has only 35 calories, 8 grams of carbs (6 g of which come from sugar), and small amounts of B vitamins, zinc, calcium, and chromium.
While Emergen-C is safe during pregnancy, as you’ll read below, you don’t want to go overboard with supplementation. As you just read, a whole food source of vitamin C is likely a better option. You’ll also notice these drink packets come with sugar; while it is not much, it is something to be aware of.
Always check the label of products like Emergen-C to verify precisely what ingredients they include.
Can I get too much vitamin C?
Since vitamin C is water-soluble, ingesting too much of this vital nutrient is difficult.
The National Institutes of Health (NIH) recommends that pregnant people consume 85 mg of vitamin C daily, with an upper limit of 2000 mg for all adults. Supplementing with over 2000 mg of vitamin C daily is not advised.
The NIH also outlines headaches, cramping, diarrhea, and nausea as side effects of too much vitamin C in one day. There is no concrete scientific evidence for overdoses causing peptic ulcers or vitamin B12 deficiencies, only anecdotal cases (26).
The Bottom Line
- Vitamin C has many essential roles in the body, including supporting the immune system, producing collagen, aiding wound healing, enhancing iron absorption, protecting against oxidative stress, and supporting the nervous system and stress response.
- Vitamin C supports fertility in both males and females—it helps boost progesterone production, improve egg and sperm quality, and support implantation and hormonal balance.
- During pregnancy, vitamin C is crucial for immune support, healthy fetal growth, and reducing the risk of complications like gestational hypertension, preeclampsia, and low birth weight. It also enhances iron absorption, especially from plant-based sources.
- In the postpartum period and while breastfeeding, vitamin C helps with recovery, wound healing, mental wellbeing, and boosting antioxidant levels in breast milk, which may reduce the risk of allergies in infants.
- Most people meet their needs through diet and a prenatal vitamin, but whole-food sources like acerola or camu camu are ideal for supplementing. Avoid high-dose synthetic supplements unless recommended, as excessive ascorbic acid can interfere with copper and B12 absorption.
Written by: Ryann Kipping, MPH, RDN, LDN, and Claire Gilmore, MSCN, CNS, LDN
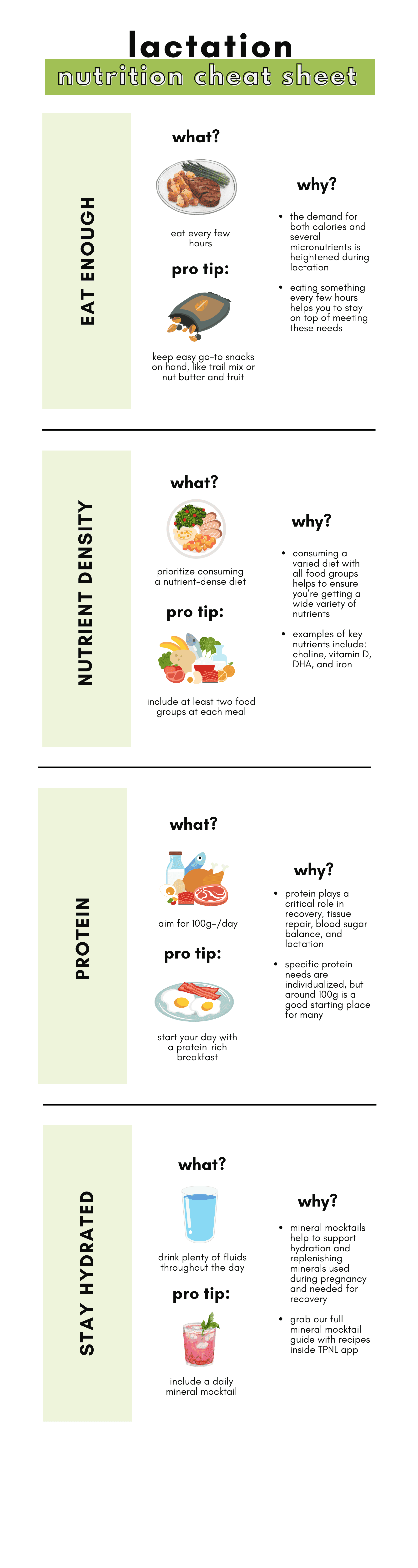
Postpartum Weight Loss

During pregnancy, your body will grow and change to support the growth and development of your little one. Despite many traditional societal pressures and messaging to “bounce back” as quickly as possible, remember you need time to heal.
Your body has undergone a remarkable transformation to create something so special, which should be celebrated. First, take plenty of time and space to focus on replenishing nutrients and bonding with your little one before delving into weight loss if this is a goal of yours.
While navigating the postpartum period, it’s very common for women to start wondering about weight loss. The amount of gestational weight gain varies largely from person to person and can be a very personal and sensitive topic.
How long is postpartum?
In its simplest definition, the postpartum period refers to the phase that follows childbirth. It begins after the delivery of your baby.
The question is, then, how long is postpartum? Or when does postpartum end? You may have heard the guidance of six weeks for a vaginal delivery and eight weeks for a cesarean section (1). Others may extend this time a bit further to 12 weeks, or what is often referred to as the fourth trimester (2).
If you’ve given birth before, you may agree that this is part of what sets many women up for the pressure and expectation to be rapidly back to their pre-pregnancy selves physically and emotionally. The truth is, this can take months or even a year or more. In fact, a postpartum depression or anxiety diagnosis can occur up to a year after birth.
When we discuss postpartum care inside The Prenatal Nutrition Library, we include the first six to eight weeks, but also extend this discussion beyond this time and well into the first year or more after birth.
Postpartum weight loss patterns
Just like weight gain during pregnancy varies from person to person, weight loss patterns during the postpartum period are also very individualized. No one loses or gains weight in exactly the same way.
Several variables, including pre-pregnancy weight, weight gain during pregnancy, whether breastfeeding or not, hormonal health and balance, metabolism, sleep patterns, and genetics, will influence weight loss patterns after pregnancy. Some of these variables are within our control, and some are not.
- Pre-Pregnancy Weight: People in a larger body size pre-pregnancy tend to retain more weight postpartum (3, 4). Research also suggests that women who had an underweight or low body mass index (BMI) before pregnancy may be more likely to retain weight initially in postpartum (5). This could possibly be a protective mechanism by the body to replenish nutrient and energy stores and support recovery.
- Weight Gain During Pregnancy: Gestational weight gain above the Institute of Medicine (IOM) recommendations during pregnancy has been identified as a predictor of postpartum weight retention initially, at one year postpartum, and beyond (6, 7, 8).
- Breastfeeding: Breastfeeding burns high amounts of calories (9). Some studies have found slightly greater weight loss at three months postpartum among mothers who exclusively breastfed compared to those who did not (10). However, nursing also coincides with increased calorie needs, as well as higher appetite and hunger levels, for most mothers (11), particularly in the early months of nursing. The impact of breastfeeding on postpartum weight loss amounts and rates seems to be individualized, as research results overall have been mixed (12, 13, 14, 15).
- Hormone Health and Balance: Pregnancy and childbirth can cause changes in hormone health and balance. For example, postpartum thyroiditis is a fairly common condition during this phase (16). Disruption and changes to hunger hormones, progesterone, estrogen, and prolactin may also impact weight loss.
- Metabolism: Metabolic rate, or the amount of calories your body burns, varies from person to person.
- Sleep: We know a quality and restorative night of sleep can be hard to come by in the early stages of postpartum and even longer, depending on the sleeping habits of your unique little one. Both lack of sleep and disrupted sleep can impact our hormones, appetite, cravings, and weight loss and gain (17, 18).
- Genetics: Genetics can impact how easily and where our bodies store weight. This can make weight loss either more or less challenging.
How long does it take to lose weight gained during pregnancy?
The time it takes to lose weight gained during pregnancy varies widely, depending on the individual and factors mentioned above, as well as overall nutrition and activity level (19).
In general, after delivery, you can expect to lose about 10-12 pounds immediately, which includes the baby, placenta, and some amniotic fluid. It is sometimes unexpected, but your belly will not immediately shrink down after having a baby.
Some additional weight loss will continue naturally in the first several weeks as the body sheds excess fluid retained during pregnancy.
Research varies significantly in terms of how long it takes to lose weight after giving birth. One study found that 60% of women returned to their pre-pregnancy weight by one year or twelve months postpartum, while another suggested that up to 75% of women were not at their pre-pregnancy weight within the same time frame (20, 22).
With the implementation of intentional nutrition and exercise interventions, a greater percentage of women return to pre-pregnancy weight within one year postpartum (54).
How long after delivery can you start trying to lose weight?
It takes around 40 weeks to grow a human, yet there has traditionally been a considerable societal pressure to ‘bounce back’ after delivery as quickly as possible.
The truth is, it takes time to heal, recover, and feel like your new, improved version of yourself again. That can be challenging to hear, and there’s no right or wrong way to feel about it. It’s very normal to feel mixed emotions about your postpartum body.
It’s absolutely okay to have a weight loss goal. However, it is essential to prioritize recovery and healing above all else. Don’t forget to celebrate the fact that your body grew an entire human from scratch. Your body has changed, and it has done this to create something truly amazing.
The amount of time each person needs to heal and recover before initiating intentional weight loss efforts varies from person to person.
In general, we’d recommend waiting until at least three months postpartum before focusing on intentional weight loss. After this time, some women begin to feel physically ready and have a more established routine.
Losing Weight While Breastfeeding
When weight loss is a goal, we need to balance adequate nutrition to support milk supply with the strategies that aid weight loss or body composition changes.
Does breastfeeding help with postpartum weight loss?
Maybe, maybe not! Like most things, it depends on the individual.
It’s estimated that exclusively breastfeeding during the first several months postpartum will require and burn up to an extra 450 to 500 calories per day (23, 52). Theoretically, increasing the calories burned should aid in weight loss.
However, research results comparing postpartum weight loss in those who breastfed with those who do not are mixed (12, 13, 14, 15, 49).
Nursing typically coincides with an increased appetite, especially in the early months. Anecdotally, many women report they couldn’t lose “the last 10 pounds” until nursing was weaned.
Will losing weight while breastfeeding impact milk supply?
Possibly.
Losing weight while breastfeeding could impact milk supply. Both the timing and approach to weight loss could have a significant impact on whether this occurs. Alongside frequent and thorough milk removal or feedings, it is essential to consume adequate amounts of calories and nutrition to support milk supply if weaning is not your goal.
Waiting until breastfeeding and milk supply are well established and regulated, even until your baby has begun to incorporate some solid foods around six months of age, is advisable for some individuals, especially if low milk supply has been a concern.
A sudden drop or significant calorie restriction may result in dips in milk supply. A very low-carbohydrate diet may also decrease milk supply, but hydration status and overall calorie consumption still play a role (25, 53).
Alternatively, a more gradual approach to weight loss postpartum while breastfeeding is generally okay. After breastfeeding is well established, a gradual weight loss of up to about one pound per week does not appear to negatively impact milk supply (24, 26). Of course, this is always individual.
Don’t forget to work with a certified lactation counselor if you have concerns about milk supply. They are invaluable resources on the breastfeeding journey.
Gentle Weight Loss Support During Postpartum
It’s okay to want to lose weight or change body composition. A healthy body composition supports overall health and decreases the risk of chronic disease (27).
However, the approach to achieving a weight loss goal is important. Postpartum weight loss should be approached in a way that allows space for healing and does not sacrifice mental well-being.
When realistic and sustainable habits and behaviors are implemented to lose weight, these changes can support mood, energy levels, and hormone health. If weight loss is done through very restrictive measures, this can lead to negative impacts on mental health and hormone health, as well as nutrient deficiencies and cycles of weight loss and regain.
There is indeed no one-size-fits-all approach to weight loss during postpartum or outside of this time, but the following are great foundations for everyone to consider.
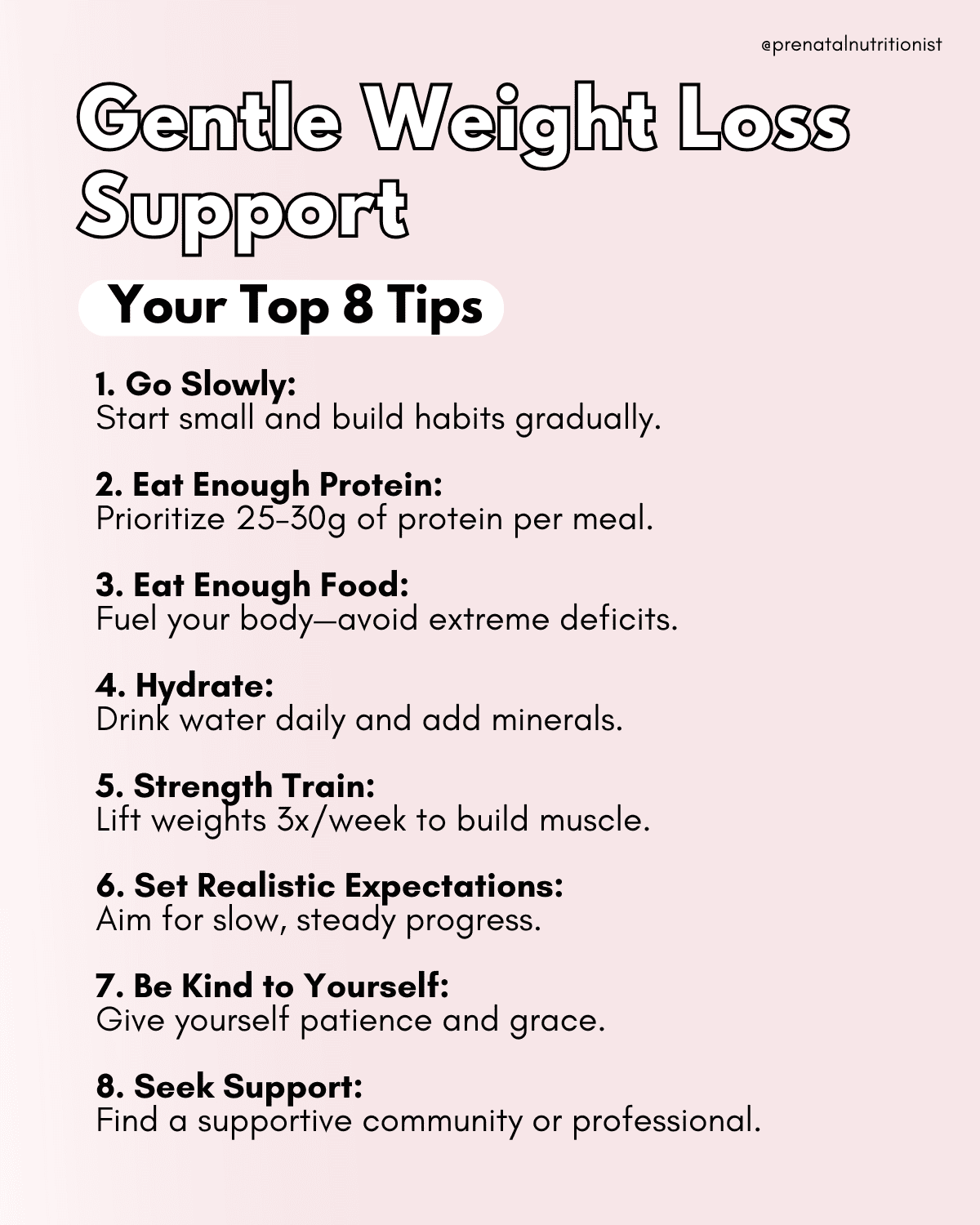
Tip 1: Go Slowly
First and foremost, before beginning an intentional weight loss goal, wait until you are physically, mentally, and emotionally ready. When you are ready, gradually incorporate habit shifts that support weight loss.
Attempting an overnight complete lifestyle overhaul rarely sticks. Often, when someone says, “I’m going on a diet,” that inevitably means that, at some point, they will come off of it. Usually, the need to “go off the plan” arises because there are restrictions that don’t leave room for the flexibility needed in life. Especially life with a little one! Your routine should leave room for “life,” like a sleepless night, illness, forgetting a packed lunch, or the human desire and experience to go out and enjoy a favorite treat.
Alternatively, consistency with small goals that build upon each other and habit stacking are valuable concepts to implement. This will look different for everyone.
One example could be starting with a goal of having a daily breakfast that contains at least 30g of protein. Once this goal is consistently achieved, your next goal may be to incorporate 20-minute walks into your routine most days.
While it may sound simple, these are the types of foundations that will make a significant impact when consistently applied.
Weight loss and maintenance of weight loss happen when these types of habits are consistently integrated into your daily life.
Tip 2: Eat Enough Protein
Protein is a key macronutrient for supporting weight loss. Of course, we also need our other two macronutrients and plenty of fiber, but protein is one that many people are under-consuming, especially when it comes to weight loss.
Protein supports metabolism, maintains balanced blood sugar levels, and promotes lean muscle mass. Additionally, eating enough protein will keep you feeling more satiated, AKA less “hanger” and cravings.
We don’t necessarily recommend tracking macronutrients or calories because there’s no need to fixate on an exact number or track every gram you consume. With that said, it’s helpful to have some idea of what you’re shooting for with protein.
Each person’s protein needs depend on individual factors such as activity level and body size. The recommended dietary allowance (RDA) for protein is 0.8 grams of protein per kilogram of body weight.
However, this is the minimum amount of protein recommended to meet basic nutrition requirements. It does not take into account activity level and is not specifically designed for weight loss or postpartum care.
Most postpartum women aiming to lose weight would benefit from consuming at least 100g of protein per day, or approximately 25-30g of protein per meal. Alternatively, a calculation of 1.6 grams of protein per kilogram of body weight can be used to estimate protein needs (28, 29).
Tip 3: Eat Enough Food
Yes, a calorie deficit is essential for weight loss, but the goal is to create the smallest deficit, or the “minimal effective dose,” needed to see progress. For lasting, sustainable results and improved body composition, it’s just as important to support your metabolism by prioritizing enough protein and building lean muscle along the way.
Major caloric deficits, or undereating, leave us at risk for nutrient deficiency and will eventually slow down basal metabolic rate (30, 31). Undereating refers to not consuming enough calories or nutrients to meet basic energy and nutrient needs.
We need to eat enough calories to support ongoing recovery, hormone health, and continued progress with weight loss. The amount of calories each person needs will depend on multiple individual factors, including activity level, height, nursing status, age, and body weight.
The Dietary Reference Intake (DRI) recommendation for adult females is 2,000 to 2,200 calories per day (32). The Dietary Guidelines for Americans (DGAs) recommendations for adult females are based on activity level and range from 1,800 to 2,000 calories per day for sedentary individuals and 2,200 to 2,400 calories per day for active individuals. Additionally, the DGAs recommend 450 to 500 additional calories per day when nursing (33).
Again, we don’t necessarily recommend tracking calories or macronutrients. Tracking food intake can contribute to unhealthy obsession over food decisions and lead to feelings of guilt for some individuals. It may take the enjoyment out of eating, and food should be enjoyed!
For those with a history of disordered eating, tracking intake may lead to unhealthy behaviors and thoughts. It’s a very personal decision whether or not tracking calories would work for you or impact your mental well-being.
With that said, we don’t generally recommend falling below 1,800 calories per day when losing weight postpartum.
Within the discussion on calories, diet quality is another important topic. Consuming a variety of whole foods and a balanced mix of protein, fat, and fiber will have a significantly different impact on our health, hunger levels, and weight loss journey than a diet lacking in these essential nutrients.
Tip 4: Hydrate
We lose water through breathing, sweating, talking, and urinating. It’s essential to replenish water and fluids throughout the day, every day. More fluids are needed when exercising as well.
Maintaining adequate hydration and preventing dehydration supports both metabolism and digestive health.
In addition to water, consider incorporating mineral support with a daily mineral mocktail. Minerals are essential for thousands of reactions and body processes, including the functioning of our metabolism, which converts the food we eat into energy (34).

Tip 5: Strength Train
There are many long-term and short-term benefits to strength training. Strength training can help us live longer and healthier lives (35). It is also a valuable component of any weight loss program.
Strength training helps to build and maintain lean muscle mass. The more muscle we have, the more calories we will burn at rest (36).
It’s also essential to understand that strength training typically doesn’t lead to significant weight loss on the scale. However, with consistency and progressive overload, it can significantly improve body composition and help maintain weight loss over the long term (37).
Body composition refers to the percentage of fat mass and lean mass (or fat-free mass) in the body. Lean mass encompasses everything except fat mass, including bones, muscles, and organs.
Once you both feel ready and are physically cleared to begin exercise, work with a post-natal certified fitness professional on an appropriate strength training program.
Tip 6: Set Realistic Expectations
Although this can vary widely from person to person, on average, it takes at least several months to one year to return to pre-pregnancy weight with intentional efforts.
Although it may sometimes be easier said than done, it’s essential not to rush the process and to acknowledge that it will take time.
In general, we do not recommend striving to lose more than about one to two pounds per week (39). Aiming for weight loss that regularly exceeds this rate could set you up for disappointment and lead you down the path of nutrient deficiency and a decrease in milk supply if you’re nursing.
Also, remember that weight loss is often not a linear process. You will likely find that some weeks you don’t lose weight, and the following week you do the same thing, and you do. That happens and is both normal and expected.
Remember that consistency and sustainability are key to success.
Tip 7: Be Kind to Yourself
Above all else, be kind to yourself. Remember, you just brought a new human into the world. There is a great deal of change and newness happening! This is true whether you’re two weeks, two months, or one year postpartum.
Negative self-talk will not help you achieve your goal faster. Postpartum weight loss is a gradual process that requires patience and consistency.
Being kind to yourself reduces pressure and supports mental well-being and a more positive body image.
Tip 8: Seek Support
Support is a game-changer for any goal we’re working towards in life. Those who have support are more likely to reach weight loss goals and maintain weight loss (39).
Support may come from friends, family, community, or certified and knowledgeable professionals in the field, such as a dietitian (hey!), personal trainer, or physical therapist.
For more personalized support from our team, explore the nutrition services we offer under the “Nutrition Services” tab!
Common Challenges and Considerations
During postpartum, you’re navigating recovery, the addition of a new family member, new routines, and more. Many variables impact the process of losing weight when this is a goal.
Lack of time and energy
Whether it’s your first or fourth child, welcoming a newborn changes the routine and dynamic of your daily life. There are often sleepless nights and days filled with diaper changes, bottle washing, and all that comes with caring for your little one.
Do your best to avoid an all-or-none way of thinking. You don’t have to do it all right from the start. Small changes add up. If you have time for only prioritizing a quality breakfast with protein, start there! It doesn’t have to be a complete overhaul of diet, exercise, sleep, stress, and all the lifestyle changes right out of the gate, or nothing at all.
Additionally, use food “shortcuts” or conveniences that make your life easier, where possible. For example, options like frozen vegetables, rotisserie chicken, pre-made hard-boiled eggs, and bagged greens. If purchasing these saves you time, that’s great.
One final tip is that we know meal prep or batch cooking is helpful, but make it work for you. It doesn’t need to be each day and all day’s worth of meals prepped for the week on Sunday. It could be as simple as washing produce for the week so it’s easily accessible, or making an extra portion of a meal when you have time to cook for leftovers the next day, or freezing it for another day.
Thyroid conditions
The pregnancy and postpartum journey can lead to changes in hormone and thyroid health (40). Postpartum thyroiditis is a relatively common postpartum condition (41). It is characterized by transient thyroid dysfunction in the first six months to one year after delivery.
Thyroid health impacts metabolism and weight loss patterns (42). Symptoms of thyroid dysfunction could include weight loss or gain, fatigue, feeling cold, muscle weakness, and constipation.
Mental health
Your mental health is most important. Movement and nourishing foods high in nutrients like omega-3s, magnesium, and B vitamins can support mental health (43).
However, if it isn’t helping you at this moment, do not prioritize weight loss over your mental well-being. It is okay if you don’t have the emotional or mental space to think about a nutrition or exercise goal of any magnitude. These can always serve as goals to revisit later on.
Prioritizing your mental health and self-care can have a profoundly positive impact on your overall well-being in numerous ways.
If you feel you could benefit from additional support for anxiety, depression, or other symptoms during this time, reach out to a professional who can offer you additional coping skills and support. You deserve to feel your very best, both for yourself and your baby.
Common ‘Mistakes’
There’s no one best set of exercises, meal plan, or macronutrient recommendations for every person. However, there are a few things to avoid to help make supporting weight loss smoother.
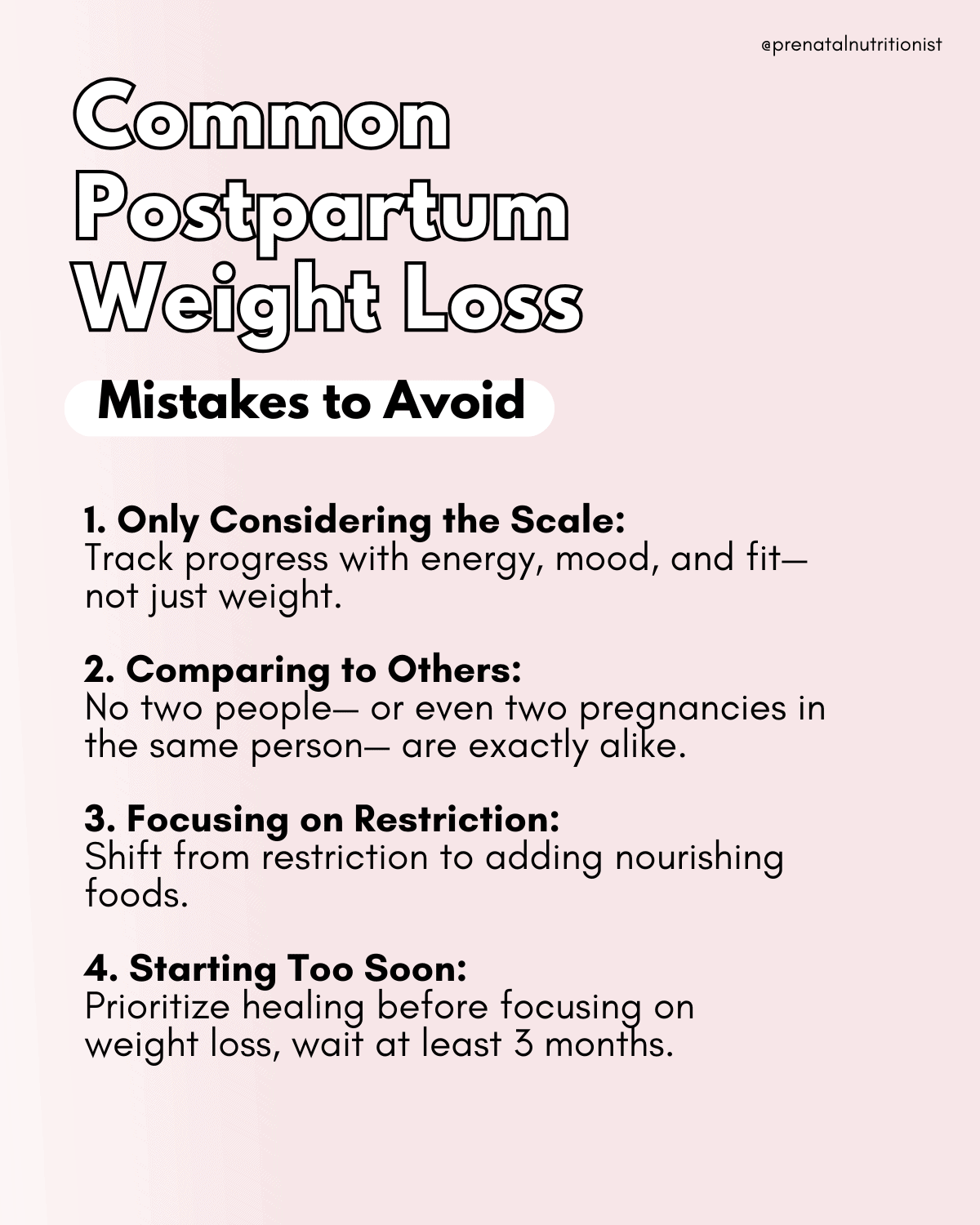
Mistake 1: Only considering the number on the scale
The number on the scale doesn’t provide a complete picture of your health or your body composition. This number doesn’t define you.
Weight is one measure, but there are so many other variables to consider. Even if weight loss is a goal of yours, that doesn’t mean you need to weigh yourself.
Use multiple markers to measure progress toward your personal goals, including how you feel, your energy levels, your mood, and how your clothes are fitting. Other technical measures, like body measurements or body fat percentage testing, are available if that interests you.
Just as counting calories is a very personal matter, so is this. We don’t recommend these types of measures if they bring up negative thoughts, worries, or obsessions for you.
Mistake 2: Comparing your postpartum journey to others
The urge to compare ourselves to others is so common. You are not alone if you resonate with this.
The thing is, every postpartum journey is so unique. Each person has a different experience with postpartum sleep, feelings, and recovery.
Do your best to resist the urge to compare yourself to others or even to your pre-pregnancy self. Your body and life have undoubtedly changed through pregnancy and the welcoming of your new little one. Take it one day at a time and prioritize your mental well-being.
Mistake 3: Focusing on restriction
Restricting calories and food groups is often the sole focus of traditional weight loss programs. However, this often leads to the “I’ll start again on Monday” cycle.
A sustainable way of eating for both health and weight loss allows room for flexibility and your favorite foods. If we continue to focus solely on what to take away, we are often left feeling deprived.
All food groups can fit into a nourishing diet that supports weight loss goals. Instead of a restriction mindset, try shifting towards an addition mindset. Ask yourself questions like, “What can I add to my plate to make this a more nourishing meal?” For example, adding vegetables, increasing protein, or starting daily walks versus eliminating sugar, bread, and cookies.
Mistake 4: Starting too soon
Throughout the postpartum period, particularly in the early stages, the primary priorities are bonding, healing, recovery, replenishment, and nourishment.
Childbirth, whether vaginal delivery or via cesarean section, involves significant physical demand from your body. If we haven’t emphasized enough, you need time to recover and heal. Jumping into weight loss efforts too soon could lead to physical injury, nutrient depletion or deficiencies, and declines in milk supply if nursing. Putting pressure on yourself to rapidly ‘bounce back’ can also negatively affect mental health and lead to added stress (44).
During the fourth trimester, also known as the postpartum period, providing your body with the space and nourishment it needs to heal and adjust is crucial. Believe it or not, it will put you in a better physical, hormonal, and emotional state when you’re ready to focus on weight loss efforts in future months, if you give your body the space to heal.
Everyone is on a different timeline for healing, but waiting at least three months postpartum before embarking on intentional and gradual weight loss would be encouraged.
Resources for Postpartum Exercise
Exercise positively impacts our overall health. It is also a beneficial component of any program aimed at weight loss or altering body composition.
Research supports that the combination of exercise and nutritional modifications effectively facilitates weight loss postpartum and helps return to pre-pregnancy weight (50, 51). Exercise burns calories, builds muscle, boosts mood, and improves insulin sensitivity.
After giving birth, it is essential to wait until your healthcare provider gives you the “green light” before starting an exercise routine or program. Be sure to also listen to your own body. If you’re exhausted, doing 60-minute super high-intensity workouts will likely do more harm than good.
Wait to start exercising until you have both been cleared by your doctor and you feel physically ready to do so. When you’re ready to start, begin slowly and ease in. Pelvic floor exercises and deep abdominal work are often recommended.
Exercise combined with healthy nutrition habits can positively support weight loss during the postpartum period. The American College of Sports Medicine recommends accumulating about 150 minutes per week of cardio exercise and at least two days per week of exercises targeting muscle strength for general health and wellness (54).
Diastasis Recti
Diastasis recti is the technical terminology for abdominal separation during and after pregnancy. The rectus abdominis muscles in the front of the abdomen stretch as the uterus grows and spreads apart during pregnancy.
The estimates of prevalence vary from about 30-45% of women experiencing some degree of diastasis recti at six months postpartum (46, 47).
It may cause or contribute to symptoms including a bulge that appears just above or below the belly button, softness around the belly button, pain during intercourse, constipation, abdominal weakness, pelvic floor weakness, urinary leaking with sneezing, coughing, or laughing (48).
Repairing diastasis recti may require targeted exercises to strengthen the deep abdominal or core and pelvic floor muscles. Work with a certified and knowledgeable exercise professional for specific guidance and exercises.
Pelvic floor exercises and physical therapy
Urinary leakage and pain are not uncommon complaints from women who have given birth. Pelvic floor exercises and physical therapy can help with recovery and lay the foundation for progressing your exercise regimen safely and pain-free.
Pelvic floor physical therapy and exercise help strengthen the pelvic floor muscles and improve their function. And it goes far beyond guidance to just “do your kegel exercises.”
 Resources
Resources
- Mamaste Fit
- Expecting and Empowered
- Get Mom Strong (Use code: RYANNPRENATAL for a 31-day free trial)
- Deliciously Fit and Healthy (Diastasis Recti Program)
- The Female Athlete (Pelvic Floor Physical Therapy Programs)
- BIRTHFIT Postpartum Programs
The Bottom Line
- There has traditionally been a large societal pressure to return to pre-pregnancy weight very quickly after birth. This does not support mom’s healing or mental well-being. Celebrate all that your body has done over the last year, and allow for plenty of time to heal, recover, and bond with your little one.
- Weight loss patterns during the postpartum period are individualized and depend on various factors, including pre-pregnancy weight, gestational weight gain, hormonal health, metabolism, sleep patterns, and genetics. No one loses or gains weight in exactly the same way.
- Everyone will be on their own timeline, and it is essential to prioritize your healing first and foremost. We generally recommend waiting at least three months postpartum before focusing on intentional weight loss efforts. Additionally, if you are nursing, wait until breastfeeding is well-established to avoid dips in milk supply.
- If weight loss is a goal of yours, aim for a gradual weight loss of about one pound or less per week. Support weight loss by incorporating nourishing and healthful habits, including daily movement, regular strength training, adequate protein intake, and plenty of fluids and hydration support.
- If you are having difficulty losing weight postpartum, despite consistently implementing positive nutrition and lifestyle habits, consider working with your healthcare team. Changes in hormone health, especially thyroid health and function, can impact metabolism and the ability to lose weight.
- Above all else, give yourself grace and prioritize your mental well-being.
Written by: Jorden Edinger, MS, RDN, LDN
Reviewed/edited by: Ryann Kipping, MPH, RDN, LDN
Vitamin B5, Pantothenic Acid
Artichokes
Apple Cider Vinegar
Breastfeeding Troubleshooting
Vitamin B2, Riboflavin
Nutrition for C-section Recovery
Lactation Cheatsheet
Hibiscus
Protein Bars for Pregnancy
Chicory Root
Yogurt
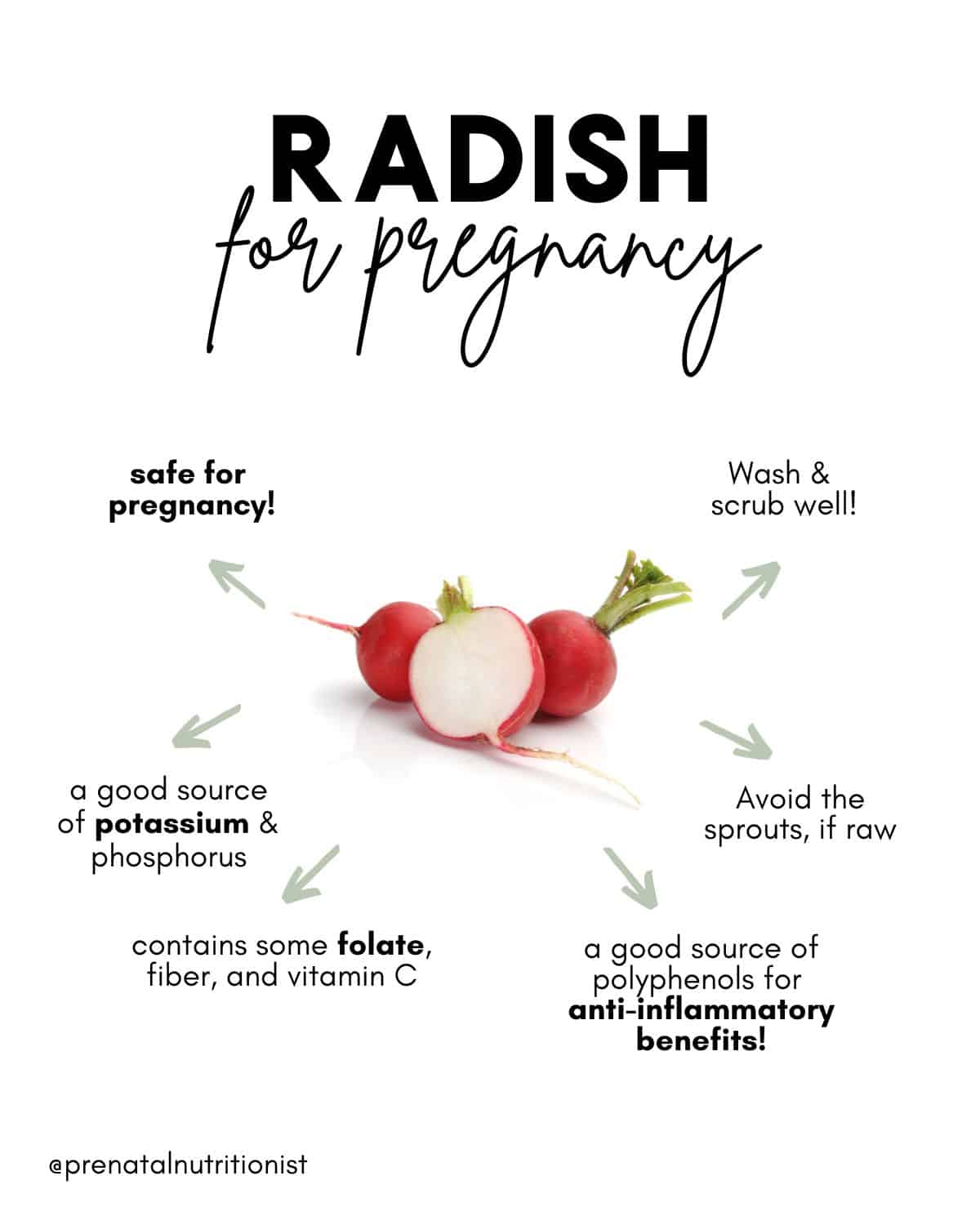
Radishes

Radishes are root vegetables, along with other veggies such as beets, carrots, rutabaga, and turnips. There are many different types of radishes, such as daikon radish, French Breakfast, Green Meat, Cherry Belle, Watermelon, Malaga (yes, these are all real varieties!), etc. They all come in different shapes, sizes, and colors!
You can almost always find the popular ‘red radish’ at the grocery store, but some of the others may be more seasonal and likely found at Farmer’s Markets. Like squash, some grow better in the winter and others in the spring. So really, you can find different varieties of radishes all year round!
Are (all) radishes safe to eat during pregnancy?
Mostly, yes!
One concern with radishes is that they (like other root crops) are said to be at a higher risk of being grown in soil contaminated with Toxoplasma gondii, which are parasites that can cause toxoplasmosis, which is a dangerous infection in pregnancy (1, 2). This infection can lead to developmental problems, miscarriage, or even stillbirth.
However, washing radishes thoroughly is one way to reduce this bacteria, as well as others, which can contaminate a raw radish during processing.
As long as you wash radishes well before eating, you can eat them (along with other root crops) while pregnant. We will go over a few more safety precautions in the section after next!
What about radish sprouts??
As with all sprouts, it is ideal to avoid raw radish sprouts during pregnancy since they carry a high risk of being contaminated with Salmonella, Listeria, and E coli.
Therefore, radish sprouts should only be eaten if they are thoroughly cooked by steaming, boiling, or baking. Wash and cook radish sprouts until 165 degrees Fahrenheit; this way, they can be safely eaten during pregnancy.
What safety measures should I take before eating radishes?
Before eating radishes, it’s recommended that you implement these safety measures as an extra means of caution before consuming: (3)
1. Scrub and wash the radishes thoroughly under running water, ideally with a vegetable brush, before eating them. A ‘produce wash’ is not necessary.
2. Cut off any bruised, browned, or damaged areas as these are areas known to breed bacteria. Discard any radishes that look overly brown.
3. If you are concerned about raw radishes, cooking them will further reduce the risk of making you sick. You can cook them by steaming and cooking them or adding them to soups, stews, sauteed dishes, or baked goods. See the last section for recipe ideas!
 Nutrient breakdown of radishes
Nutrient breakdown of radishes
½ cup radishes, raw (58 grams) (USDA)
Energy: 9.23 kcal
Protein: 0.4 g
Total fat: 0.1 g
Carbs: 1.97 g
Fiber: 1 g
Calcium: 14.5 mg
Magnesium: 5.8 mg
Phosphorus: 11.6 mg
Potassium: 135 mg
Vitamin C: 8.6 mg
Folate: 14.5 ug
What benefits do radishes have for pregnancy?
Polyphenols. Radishes are rich in non-flavonoid polyphenols and glucosinolates (4). These compounds provide anti-oxidative and anti-inflammatory benefits to repair damaged cells and lessen conditions associated with increased oxidative stress, including miscarriage and preeclampsia (5, 6).
Potassium is an essential mineral and electrolyte that supports normal fluid balance, hormone production, protein formation, heart function, and blood pressure.
Vitamin C is not only essential for supporting immunity and skin health, but Vitamin C plays a vital role in the development of the fetus’s brain. It also helps regulate blood sugar and support collagen synthesis (7, 8).
Vitamin C also helps regenerate vitamin E, another vitamin that acts as an antioxidant (9).
Phosphorus. Getting enough phosphorus is necessary to support your baby’s skeleton development, cell function, and regulation of blood sugar levels (10). Not getting enough phosphorus during pregnancy has been associated with an increased risk of preeclampsia (10). A ½ cup of raw radishes provides almost 12 mg of phosphorus to contribute to your daily intake.
A small amount of fiber. Radishes provide some fiber (1.6 grams per 100-gram serving) to help meet your daily recommended intake of 30 grams per day during pregnancy.
I include radishes in my pregnancy diet?
Radishes do not have a strong flavor but can add a colorful crunch to many dishes! As discussed at the beginning, there are so many radish varieties to choose from, so get creative, and try to venture out of your comfort zone.
Ideas for including radishes in your daily meals and snacks include:
- Sliced over salads
- Sliced on top of avocado toast
- Dipped into hummus, pesto, or tzatziki
- Mixed into greek yogurt with cucumbers and dill
- Baked as radish chips
- Baked with butter on a baguette
- Roasted and dipped in ranch
- Sauteed with bacon
The Bottom Line
- Radishes are safe to consume during pregnancy, and with a few safety precautions, they can carry even fewer risks for you and baby.
- Scrub and wash the radishes thoroughly under running water, ideally with a vegetable brush, before eating them.
- Cut off any bruised, browned, or damaged as these are areas known to breed bacteria, and discard any radishes that look too brown. If you are concerned about raw radishes, cooking them will further reduce the risk of getting sick. You can cook them by steaming and cooking them or adding them to soups, stews, sauteed dishes, or baked goods.
- Radishes contain polyphenols, vitamin C, potassium, phosphorus, and fiber, which all support your and your baby’s health and well-being during pregnancy.
Written by: Claire Gilmore, MSCN, CNS, LDN, and Ryann Kipping, MPH, RDN, Owner + Founder
Olives
Aloe Vera
Inositol
Quick Snacks
High Cholesterol
Acai

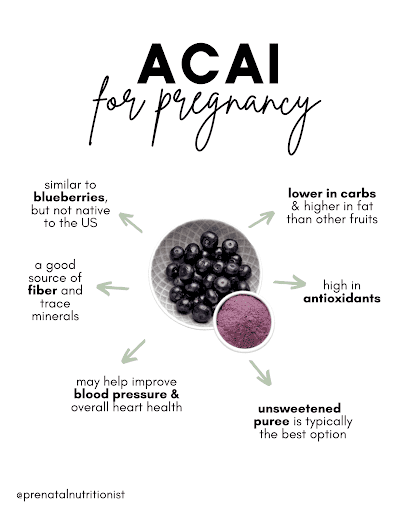
What are acai berries?
Acai berries are a fruit product that comes from the acai palm tree, native to tropical Central and South America. The fruit is a deep purple-colored berry that serves as an important food source for the indigenous people of the Amazon; and has gained popularity for its antioxidants and flavor in recent years [1, 4].
Their popularity in the US may be partly because Oprah named them a ‘superfood’ (quotes because this is not a scientific term) on her show because the acai berry contains more antioxidants than blueberries, strawberries, and cranberries [5].
The acai palm trees can grow up to 60 feet high in the Brazilian rainforest and since harvesting is done by hand, locals scale dangerous heights to harvest them [5]. These berries also spoil very quickly, so harvesting, processing, and shipping is a very fast process. This is the reason why raw acai berries are very hard to come by here in the US. While they can technically be eaten raw, they are usually consumed in the form of juices, frozen puree, smoothies, sauces, gummies, powders, and other dietary supplements.
As we talk about here often, food in its most whole form is always our the best option!
Are acai berries safe during pregnancy?
Mostly, but it depends!
According to the NIH, there is very little information known about the safety of eating acai during pregnancy or while breastfeeding [6]. However, most registered dietitian sources claim it to be safe for pregnant mamas to consume, but you’ll have to be careful about how it is prepared and aware of the potential risks.
After all, it is much like any other berry just not native to the US!
Acai Berry Nutrient Breakdown [9]
In 1 packet of acai puree:
- 60 Calories
- 2 g Protein
- 5 g Fat
- 6 g Carbohydrates
- 3 g Fiber
- 40 mg Calcium
- 1.08 mg Iron
- 7 mg Sodium
- 9.6 mg Vitamin C
- 1000 IU Vitamin A
What are the benefits of acai berries?
At this time, more research needs to be conducted on humans on the health benefits of acai products [4]. However, we can go through the current limiting research that is out there about acai and its potential health benefits.
Nutrient-dense
The nutrition profile for acai is quite unique for fruit because they are actually a little higher in fat and lower in sugar [10]. Additionally, they contain essential trace minerals like chromium, zinc, iron, copper, manganese, magnesium, potassium, and phosphorus, according to a Venezuelan study [11]!
Acai berries also contain anthocyanins – these are plant compounds that give acai their deep purple color. Anthocyanins are known to possess antidiabetic, anticancer, anti-inflammatory, antimicrobial, and anti-obesity effects [12]. Acai berries are also higher in antioxidants than other berries we commonly eat and are a good source of fiber [13].
May improve brain cognition and memory
Due to their antioxidant-rich qualities, acai berries could improve cognitive and motor functions – according to an animal study from the Journal of Agricultural and Food Chemistry [14]. Another animal study found that acai berries could protect memory during aging because of their anti-inflammatory properties [15].
May improve cholesterol levels and lower the risk of heart disease
According to an uncontrolled pilot study, eating 100 g of acai pulp twice a day for one month can help reduce cholesterol levels in overweight individuals [16]. Another study found that anthocyanins and flavonoids (such as those found in acai berries) contribute to the prevention of hypertension and subsequently, lower the risk of heart disease [17].
New research showed that acai supplementation in animal models improved maternal hypertension and reduced the chances of intrauterine growth restriction. The researchers noted this is likely due to the antioxidant content of acai.
May help decrease inflammation
An interesting study completed in rats during pregnancy found acai supplementation with the control diet resulted in improved lipid profiles, better glucose levels, and improved gut microbiota. They also noticed an improvement in inflammation in the colon among the offspring. All these benefits sound nice but remember humans are pretty different than rats.
A more recent study showed that acai intake among healthy women (yes, humans this time) had no effect on inflammatory biomarkers, but the researchers did state inflammation is a product of the diet as a whole. This we know, studying individual foods and even individual nutrients is hard due to the synergistic effect of foods, and the effect all the foods we consume have on inflammatory biomarkers.
Are there any risks to enjoying ‘acai’ during pregnancy?
Supplement and powders
Acai powder is essentially finely ground-dried acai berries, and since all the water has been removed, it is an extremely concentrated product. It’s popularly used as a supplement. The lack of research done on acai as a supplement makes it safe to advise that excess intake should be avoided during pregnancy. It’s best for pregnant mamas to stick to one serving of acai powder a day or better yet, focus on the puree packets with no added sugar as the best option.
 Acai juice
Acai juice
Acai juice is commonly added to drinks, smoothies, and the famous Starbucks Strawberry Acai Refresher which contains 45 mg of caffeine. The same rule for juices during pregnancy applies here as well, always go for pasteurized or filtered juices.
One risk of drinking unpasteurized acai juice is Chagas Disease or American Trypanosomiasis – a tropical, parasitic, life-threatening disease that can induce cardiac and digestive complications [18]. Although this disease is not common in the US (most cases have been reported in the Southern United States), it’s a good thing to consider when traveling to countries in South America, Central America, and Mexico; or if you or your family spend a lot of time outdoors in tropical areas [19].
What about ‘acai bowls’ at local shops?
One of the most popular ways we enjoy acai in the US is the trendy acai bowl. These bowls are made from a frozen acai puree as the base and then decorated with multiple toppings. These bowls are commonly offered in a thick, creamy consistency using a soft-serve style ice cream machine or out of big “ice cream” like tubs.
Are they safe for pregnancy?
The concern with any ‘soft-serve’ machine is the cleanliness. They are breeding grounds for bacteria when not properly cleaned, namely Listeria – known for their capability to cause serious complications during pregnancy, including miscarriage, stillbirth, premature delivery, or newborn infection. It’s important to remain cautious of this risk. I personally have not come across a place that uses a soft-serve machine for acai living in Southern California.
No matter the tool that is used, make sure you go to a reputable acai bowl shop that is diligent in their cleaning practices; one that you trust. You can always talk to a manager to ask about cleaning protocols. Getting your acai bowl from street vendors or at local fairs is not a good idea since they aren’t likely to have clean and sanitized equipment [20].
High in Sugar
Acai bowls are definitely a sweet treat, which is completely okay once in a while and won’t harm you or your baby. However, habitual consumption of acai bowls, especially from local shops likely with plenty of added sugar can quickly add up. A diet high in sugar that leads to excess weight gain during pregnancy can increase a pregnant mama’s risk for several unwanted pregnancy complications [21]. Learn more about sugar consumption during pregnancy here.
Ordering recommendations
To make your acai bowl a more balanced treat, consider topping it with plant-based fats and protein like hemp seeds, chia seeds, flaxseeds, dark chocolate, and nut butter.
Not only will it make your snack more delicious, but it will also make it more filling and provide you with longer-lasting sustained energy! You can take these recommendations into consideration when making acai bowls at home also. If you’re buying unsweetened frozen acai puree, you can always top it with some banana, honey, or maple syrup to sweeten it up!
Can I enjoy it if I’ve been diagnosed with gestational diabetes?
The main goal for pregnant mamas with gestational diabetes is to control their blood sugar levels. Acai bowls tend to be high in carbohydrates (the only macronutrient that significantly affects blood sugar) – from the fruit, sweeteners, and toppings. This doesn’t mean pregnant mamas can’t enjoy a nice cooling bowl of acai, but it’s important to prepare for it, and know-how to order.
Make sure you check your glucose numbers before and after to see how they are affected. It might be a better idea to share the bowl with your partner or a friend because some bowls could have up to 60 g of carbohydrates, and even more when considering toppings.
If your bowl is blended fresh, add a protein like a peanut butter, protein powder, and hemp seeds. It is also great to add these as toppings to boost the protein and fat content. In addition, you could pair it with an outside protein source like a piece of cheese, jerky, or yogurt.
What to look for when purchasing acai at the store
There are lots of acai products on the market, and it can be confusing to choose the brand that’s best for your health goals during pregnancy. We want to consider two main things – pasteurization and no added sugars. When you’re browsing your grocery store’s freezer aisle, look for acai packets that are unsweetened and acai juice that is pasteurized or filtered.
Here are a few great brands to try:
How to enjoy acai at home
How can we put this delicious treat together?
Acai bowls are fairly quick to make and require 3 components: acai berry puree, fruit, a protein (almond butter, peanut butter, protein powder), and your favorite toppings! I’ve listed a few more different ways you can enjoy acai at home for a fraction of the cost and still get all the amazing benefits of fiber, antioxidants, and healthy fats.
- Customizable acai smoothie bowls
- Acai oatmeal yogurt bowls
- Fruit salad with honey acai dressing
- Acai Smoothies
- Acai Lemonade
The Bottom line
- Acai is a berry that looks like blueberries but is not native to the US; Brazil is where they are mainly grown and harvested. While acai is safe, the research on pregnancy and breastfeeding is limited.
- Acai is high in antioxidants, fiber, and trace minerals, and is slightly lower in carbs and higher in fat than most fruits. It is best enjoyed in low to moderate amounts.
- The best options for at-home use are unsweetened acai frozen packets/purees. You can add your own sweetener when making smoothies like a drizzle of honey or maple syrup.
- Avoid acai powders and supplements during pregnancy as they are not FDA regulated nor have they been proven safe.
- If you’re going to enjoy an acai bowl at a local shop, make sure the shop is a clean, reputable place you trust that follows food safety protocols. If you can choose, the unsweetened or freshly blended option with toppings like nut butter and seeds.
Written by: Nina Cassett & Laima Numan, Dietetic Interns, and Ryann Kipping, MPH, RDN, Owner + Founder