Month: October 2020
Mushrooms

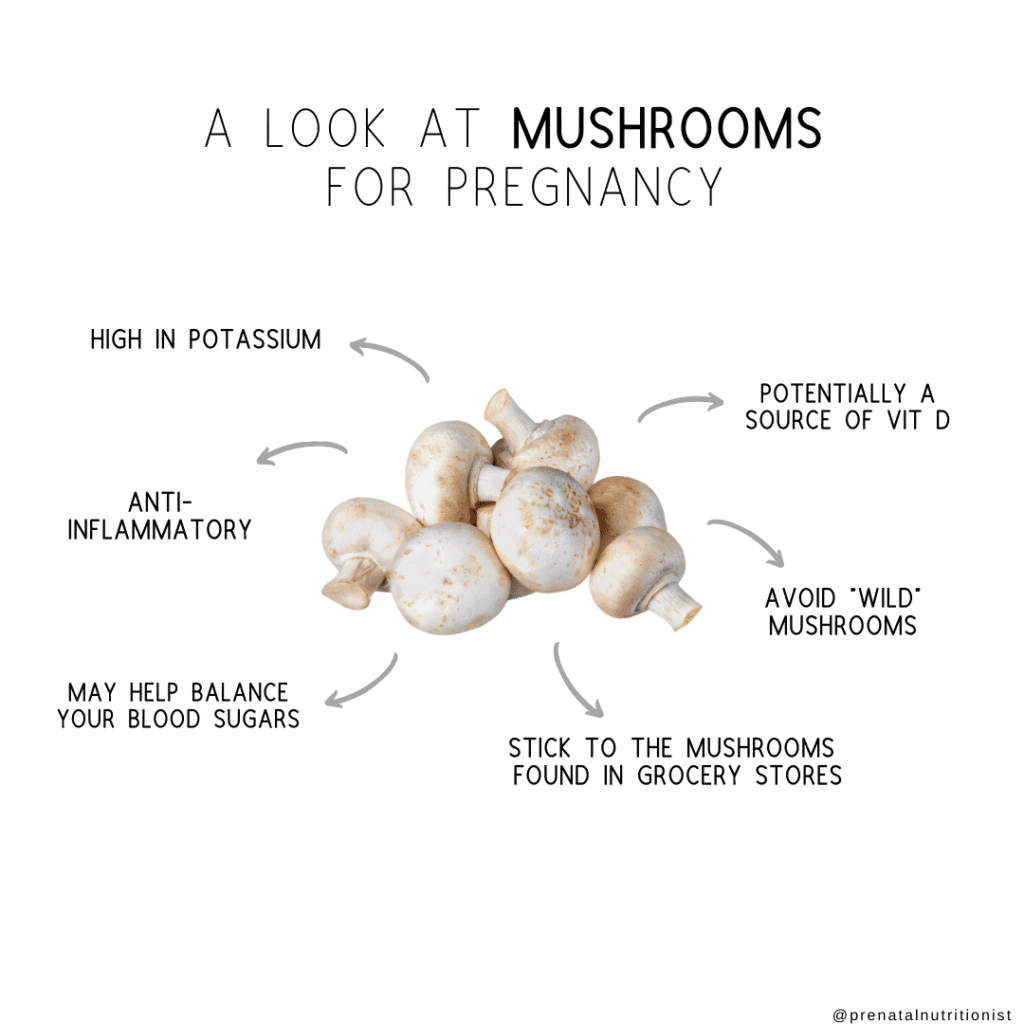
Mushrooms are often categorized as a vegetable but are really fungi. They have been used for thousands of years as medicine and in food all over the world.
You might think of this funky fungus growing wildly in the yard or passing it by on hikes, but many non-toxic varieties add flavor and nutrients to your meals.
So, can you still enjoy mushrooms during pregnancy?
We cover everything you need to know about mushrooms during pregnancy below.
Can you eat mushrooms while pregnant?
The big question is, are these fungi safe for your growing body and baby?
Well, mostly. Most mushrooms you find in grocery stores are safe to eat during pregnancy and provide plenty of benefits, too.
Which mushrooms are safe to eat during pregnancy?
- Button
- Baby bella
- Portobello
- Shiitake
- Oyster
- Cremini
- Enoki
- Porcini
- Chanterelles
When shopping for mushrooms, make sure they are firm and do not have any bruising.
While you can eat mushrooms raw or cooked, they are mainly served and eaten cooked. There is quite the debate whether we should always eat them cooked or if that denatures some of the nutritional content.
Cooking vegetables helps make them more easily digestible and also helps to eliminate any chance of bacteria lingering on the exterior.
Which mushrooms are unsafe during pregnancy?
Not all mushrooms are created equal. The “magic” kind perhaps, are of course not safe or suggested to use in pregnancy. They can cause hallucinations, muscle weakness, drowsiness, nausea, and vomiting.
Mushrooms you find in the “wild” should also be avoided. Collecting wild mushrooms poses the danger of potentially toxic mushrooms because you may not be able to properly identify them.
The side effects of eating toxic mushrooms are nausea, vomiting, and general intestinal discomfort.
There is one documented report of a pregnant woman eating an Amanita mushroom and suffering from nausea, vomiting, diarrhea, and a 5-day hospital stay, however, both baby and mom were fine (1).
Interestingly, there are some mushroom species yet to be discovered, so for now, stick to the grocery stores when it comes to purchasing and eating mushrooms during pregnancy!
Mushroom nutrition information
1 cup of white raw mushrooms, sliced (2)
- Calories: 15
- Carbohydrates: 2.3 g
- Protein: 2.2 g
- Fat: 0.2 g
- Sugar: 1.4 g
- Fiber: 0.7 g
- Potassium: 220 mg
- Selenium: 6.5 mcg
Mushrooms contain a number of vitamins and minerals that are important during pregnancy such as calcium, magnesium, potassium, and selenium.
Notably, their star nutrient is potassium. One cup of white mushrooms contains three-fourths of the amount of potassium that one banana provides.
Potassium is an electrolyte and mineral with many essential functions in the body including heart rhythm, muscle contractions, blood pressure, digestion, and more (3).
Are there benefits to eating mushrooms during pregnancy?
Gut microbiota
Mushrooms contain prebiotics which is a specific type of fiber that feeds the healthy bacteria in our gut. Research is building on how mushrooms can positively affect the balance of bacteria in our gut (4).
An imbalance of bacteria in the gut during pregnancy affects both mom and baby. Research shows this balance affects maternal weight and weight gain during pregnancy and can permanently affect the offspring’s metabolism (5).
Vitamin D
If grown in proper sunlight or UV-C radiation, mushrooms can be a source of vitamin D2, a nutrient that is limited when it comes to food sources, but vitally important for pregnancy (6).
Although it is estimated that 3 button mushrooms from your average grocery store only contains 40 IU vitamin D2 (7). When these same mushrooms are exposed to 15-120 minutes of mid-day sunlight, they will produce up to 10 times the amount of vitamin D.
For reference, one egg contains around 50 IU of vitamin D (8).
Enhancing your diet with mushrooms during pregnancy adds a crucial nutrient that up to 50% of pregnant women are deficient in (9).
Anti-inflammatory
While inflammation is a necessary response in our bodies, repeated inflammation without proper care results in chronic inflammation which is not good for our health (10). Inflammation in pregnancy has been linked to gestational diabetes and preeclampsia (11, 12).
Mushrooms contain many components that contribute to reducing inflammation.
Antioxidants such as carotenoids, tocopherols, and vitamin c, in addition to certain amino acids and fatty acids are all responsible for the anti-inflammatory properties in mushrooms (10).
Blood sugar control
There is some documentation that suggests mushrooms help control or reduce type 2 diabetes (13). While these studies aren’t specific to gestational diabetes, they showed a reduction in blood sugar levels and hemoglobin A1C, both biomarkers of diabetes in and outside of pregnancy (13).
It is important to note, many of these studies were completed in mice, but nonetheless, it appears it definitely can’t hurt to include various types of mushrooms in your diet.
Overall, mushrooms provide many benefits to our diet. A healthy gut microbiota, adequate vitamin D intake, low inflammation, and blood sugar control are all important aspects of nutrition during pregnancy.
How to add mushrooms to your diet
Vegetarians are often quick to use mushrooms since they are a great ingredient to help create the taste and texture of meat products, but others can simply use them as a topping or side dish.
- Portobello “steaks”
- Sauté with onions to top a protein of your choice
- Mushroom soup
- Roast alongside assorted veggies
- Add to pasta or pizza
- Use in an egg scramble or omelet
What about mushroom coffee during pregnancy?
Mushroom coffee is the latest and greatest energy trend, but are they safe for pregnancy?
While we could write a full article on this topic alone, it felt necessary to include a brief statement about this mushroom product here.
Mushroom coffee is black coffee with powdered mushrooms mixed in it. It contains about the same amount of caffeine as green tea, so less than your average cup of joe. Mushrooms used typically include lion’s mane, cordyceps, chaga, or reishi; no psychedelic mushrooms are used.
There is no research on mushroom coffee during pregnancy and it is important to be aware of other ingredients contained in the coffee as well. Some blends include different herbs like tulsi (14).
Adding edible mushrooms to coffee doesn’t seem like any cause for concern, but do proceed with caution verifying all ingredients and ensuring quality.
The Bottom Line
- While now is certainly not the time to be experimenting with wild mushrooms in the woods, it is the perfect time to grab your favorite kind of mushroom from the grocery store and prepare it the way you see fit.
- Including mushrooms during pregnancy may contribute to your vitamin D intake and help keep your blood sugar in check.
- Lastly, if you are not traditionally a mushroom eater, you can see there are many benefits to including them in your diet.
By Ryann Kipping, MPH, RDN, CLEC | Owner & Founder and Lauren Gannon, RD
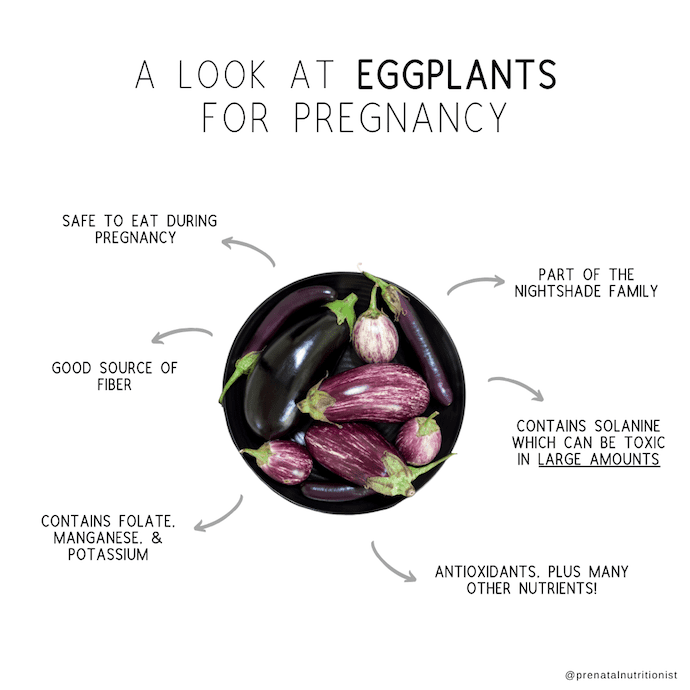
Eggplants

Eggplants during pregnancy
If you follow a Mediterranean style diet (or enjoy eggplants), you may be wondering if you can enjoy eggplants during pregnancy.
This big purple squash is classified as a “nightshade”, a group of over 2,000 plants, although few of them are actually eaten. Some other nightshades include tomatoes, potatoes, and peppers.
You may have heard eggplants are dangerous to consume during pregnancy, but is this true?
Below we will take a look at the safety of eggplants while pregnant and also, the nutrients they provide for you and your growing baby.
Is eggplant safe during pregnancy?
Yes, eggplants are safe to eat during pregnancy. However, in this case, you can get too much of a good thing.
 Nightshades such as eggplants contain a substance called solanine which can be poisonous if consumed in high quantities.
Nightshades such as eggplants contain a substance called solanine which can be poisonous if consumed in high quantities.
Solanine
Have your potatoes ever turned green?
This green color is essentially a warning that the solanine in the potatoes may be at a toxic level. Eggplants don’t come with a warning, but you would have to try really hard to overdo it.
Solanine poisoning occurs when you are exposed to high levels of solanine and can cause symptoms such as diarrhea, vomiting, fever, and/or stomach pains.
You would need to eat over 400 mg of solanine for it to be poisonous and most nightshade vegetables contain anywhere from 2-13 mg of solanine (1).
So, unless your cravings are very strong, you will be just fine indulging in that eggplant parm from your favorite Italian restaurant.
Eggplant nutrition breakdown
1 cup or 82 grams raw, eggplant (2)
Calories: 20.5 calories
Carbohydrates: 4.8 g
Sugar: 2.9 g
Protein: 0.8 g
Fat: 0.2 g
Fiber: 2.5 g
Manganese: 0.2 mg
Folate: 18 μg
Potassium: 188 mg
Benefits of eggplant during pregnancy
Antioxidant properties
You may have heard this fancy word before but what is an antioxidant and why do I want it in my diet?
Antioxidants are substances that help protect the body from free radicals or harmful substances that may be floating around. Antioxidants are helpful in the prevention of chronic diseases such as heart disease and cancer (3).
More specifically, eggplants contain anthocyanins, the antioxidant that is responsible for eggplants bright and vibrant purple color (4).
Fiber
As you read above, 1 cup of raw eggplant contains 2.5 g of fiber.
Increasing fiber intake along with fluid intake is the first line of treatment for constipation during pregnancy, but fiber has many other functions other than to keep you “regular” (5).
Fiber helps keep you full longer and slows the rate at which your blood sugar rises, truly a win, win, win.
 Folate
Folate
Eggplants contain folate, a nutrient vital for the growth and development of your baby. Inadequate folate intake has been linked to several poor pregnancy outcomes (6).
Even 20 years after the US required folic acid fortification in grain-based products, around 20% of women are still deficient (7). Adding more high folate foods to your diet pre-pregnancy and during pregnancy is wise.
Manganese
Manganese is one of the least studied micronutrients when it comes to pregnancy. Although you are unlikely to be deficient, it is still important to consume the recommended amount as both deficiency and excessive consumption can lead to negative outcomes (8).
Two studies found that both low levels and high levels of manganese during pregnancy correlated to low birth weight in offspring (9, 10).
How to include eggplant in your diet
Eggplants are a versatile ingredient. While opting for “low-calorie” food finds is generally not recommended during pregnancy, if you find yourself in a situation where you are gaining too much weight too quickly, this is a great addition to any meal.
Here are some recipe and meal ideas to incorporate eggplant into your meals:
- Eggplant parmesan
- Eggplant lasagna
- Marinated teriyaki eggplant
- Eggplant pizza
- Eggplant fries
- Eggplant “BLT”
- Roasted eggplant
The Bottom Line
- While you can eat too much eggplant, a daily serving of eggplant will not harm you or your baby during pregnancy.
- Not only is consuming eggplant during pregnancy completely safe, but it also comes with benefits!
- Eggplant provides fiber, folate, manganese, and antioxidants, amongst other nutrients important for you and baby during this time.
By Lauren Gannon, RDN and Ryann Kipping, MPH,RDN, CLEC | Owner & Founder
Low-Mercury Seafood
Pistachios
Strawberries

Strawberries are delicious and filled with vitamins. They are in season in the spring and summer, and when picked ripe, they offer a naturally sweet flavor that will surely give you a hard time putting your berry bowl away.
But, are there benefits to eating strawberries while pregnant? We have your answers right here.
Are strawberries safe during pregnancy?
Yes, strawberries are safe to eat during pregnancy!
There are major benefits to incorporating this fruit into your daily diet, which we’ll go over below, as well as some tips to make sure you’re buying the healthiest strawberries possible.
Are strawberries good for pregnancy?
Healthy food choices are critical while you’re pregnant and growing your baby.
Not only do you need vitamins, minerals, and antioxidants to keep yourself healthy and meet the demands of your body, but your baby will benefit from all of the nutrition you choose to eat.
Strawberries are filled with water, which is essential to keep yourself hydrated. As a pregnant lady, you have increased hydration needs to accommodate your growing baby.
Water helps to form the placenta and carry nutrients to your baby, this “new organ” is a pivotal piece to a healthy pregnancy and baby.
Strawberries have a few carbohydrates in them, which is what you need to have energy, but strawberries also have fiber, which is a type of carbohydrate (1).
Fiber helps to keep your bowel movements normal and maintains your bowel health. Fiber can also help to keep you fuller for longer, which makes it easier to control your weight if that’s something you’re concerned with (2).
Strawberries also have folate, which is important in tissue and cell function. This vitamin is also essential for pregnant women to consume so your baby can grow and develop normally before entering the world (3).
In lesser amounts, as you’ll see below, strawberries also contain nutrients such as potassium, phosphorus, and magnesium.
 Strawberry nutrition breakdown
Strawberry nutrition breakdown
1 cup whole strawberries (144g)
Water: 131 g
Calories: 46 calories
Carbohydrates: 11 g
Fiber: 2.9 g
Calcium: 23 mg
Iron: 0.59 mg
Magnesium: 18.7 mg
Phosphorus: 34.6 mg
Potassium: 220 mg
Sodium: 1.4 mg
Vitamin C: 84.7 mg
Folate: 34.6 ug
All values provided by the USDA nutrient database.
Vitamin C during pregnancy
Vitamin C is a vital antioxidant, and strawberries are filled with it!
Vitamin C is important for immunity and helps the absorption of iron in the body. It has been linked to birth weight and length and may even contribute to appropriate growth all the way up to six months of age (4, 5).
Read more about vitamin C in our lemons during pregnancy blog post.
Click here to read more on lemons.
I’m craving strawberries during pregnancy, is this normal?
Cravings during pregnancy are, for the most part, very normal.
A lot of women crave fruit for a variety of reasons, one being the high water content. As discussed above, fluid needs during pregnancy are heightened and your body is looking to make those extra needs up in any way it can.
Second, like many other fruits, strawberries contain folate, Vitamin C, and other nutrients that your body needs more during pregnancy.
Usually, it is okay to go ahead and give your body what it is asking for unless you have a strong urge to eat non-food items. Read more on pica during pregnancy in our previous blog on this topic.
Click here to read more on Pica
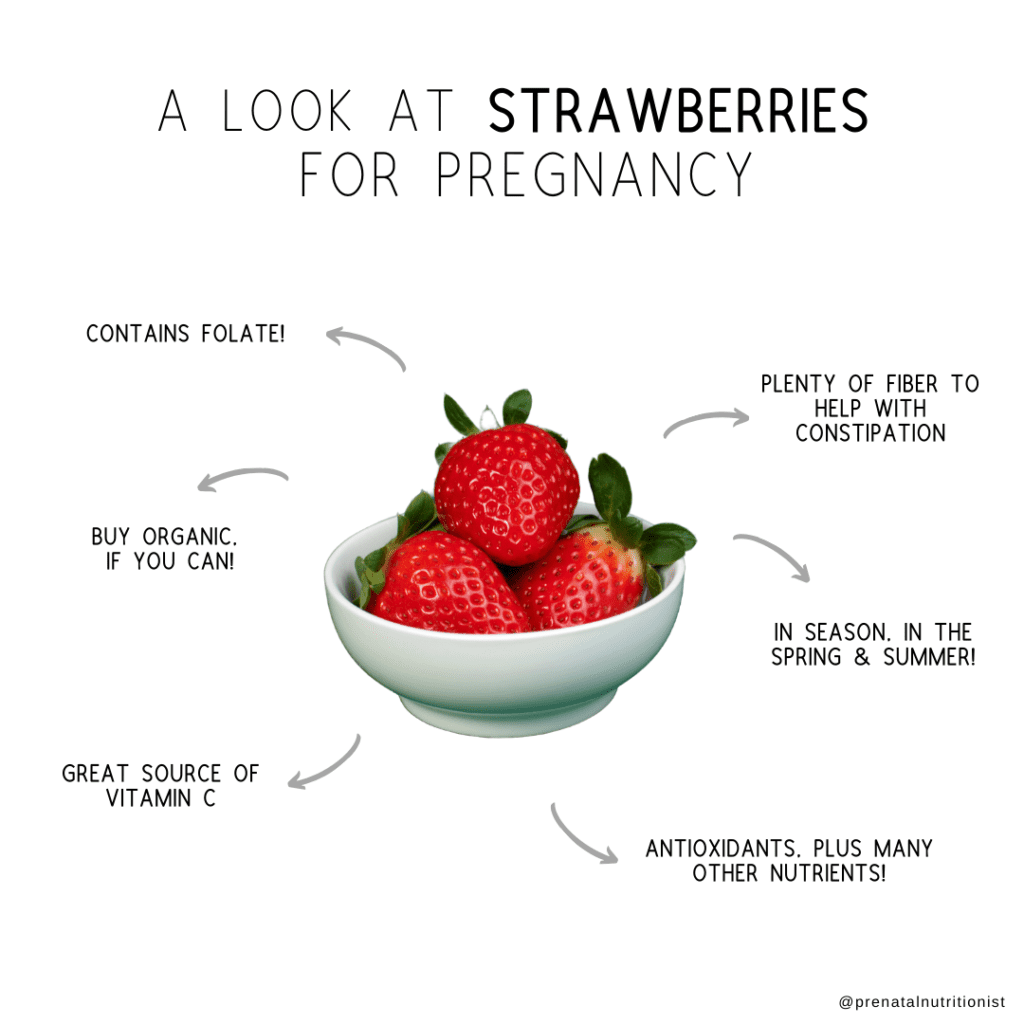
Tips for purchasing strawberries, should you go organic?
Strawberries taste best and have the most naturally occurring nutrients in them when they are in season, which is in the spring and summer.
Every year, strawberries are routinely placed on the “dirty dozen” list, which is a list of the foods that have the most pesticides on them (6). The list comes from an analysis of the United States government’s Pesticide Data Program report.
 It can be really scary to think about chemicals and pesticides and toxic substances coming into your body and potentially harming you, or your baby.
It can be really scary to think about chemicals and pesticides and toxic substances coming into your body and potentially harming you, or your baby.
While it’s very important to remember fruits and vegetables, organic or not, are extremely beneficial to consume during your pregnancy, a growing body of evidence suggests the repeated exposure to pesticides may affect pregnancy outcomes (7, 8, 9, 10, 11).
Strawberries have appeared top of the “dirty dozen” list year after year.
If your budget allows, focus on buying the “dirty dozen” list organic and saving money on the other produce. It’s wise to compare prices while at the store, you may be surprised that some organic options are the same price or even cheaper in some instances.
How to include strawberries in your diet
Strawberries, of course, taste quite delicious on their own, but there are so many ways you can enjoy them.
- In a yogurt bowl
- With whipped cream for a dessert
- Blended in a smoothie
- Dipped in chocolate
- On top of toast with ricotta cheese
- In chia seed pudding
- Slice on top of pancakes or waffles
- Top your oatmeal or have alongside eggs
Be sure to thoroughly wash your strawberries before using them just like all your other produce.
 The Bottom Line
The Bottom Line
- Strawberries are safe and healthy for you and baby while pregnant. They are packed with fantastic vitamins, and even contribute to your fluid needs for the day.
- While you cannot control the pesticides that are on the strawberries, you can choose to focus on the health benefits and their delicious taste.
- Choose organic strawberries if the thought of synthetic pesticides isn’t welcoming and if your budget allows.
By Alexa D’ Orazio, MS, RDN and Ryann Kipping, MPH, RDN, CLEC | Owner & Founder
Lemons

Does using lemons during pregnancy have benefits? Whether it be to add some flavor to your water, zest up a salad, or help with nausea, we have your lemons questions answered.
Is lemon safe during pregnancy?
Lemons as with the majority of fruits are safe to consume during pregnancy and can provide nutritional value.
They can be added to water, top salads, or to flavor baked goods.
Eating lemon during pregnancy is safe, but just like anything else, moderation is key and if you happen to be overindulging in one particular food, be sure to run it by your OBGYN, midwife, or dietitian.
Nutrient breakdown
Because it is a citrus fruit, lemons contain a good amount of vitamin C and a number of vitamins and minerals including B-vitamins, niacin, and folate (1).
One small lemon contains:
- Calories: 25 calories
- Carbohydrates: 8 g
- Fat: 0.3 g
- Protein: 0.9 g
- Fiber: 2 g
- Vitamin C: 45 mg
- Calcium: 22 mg
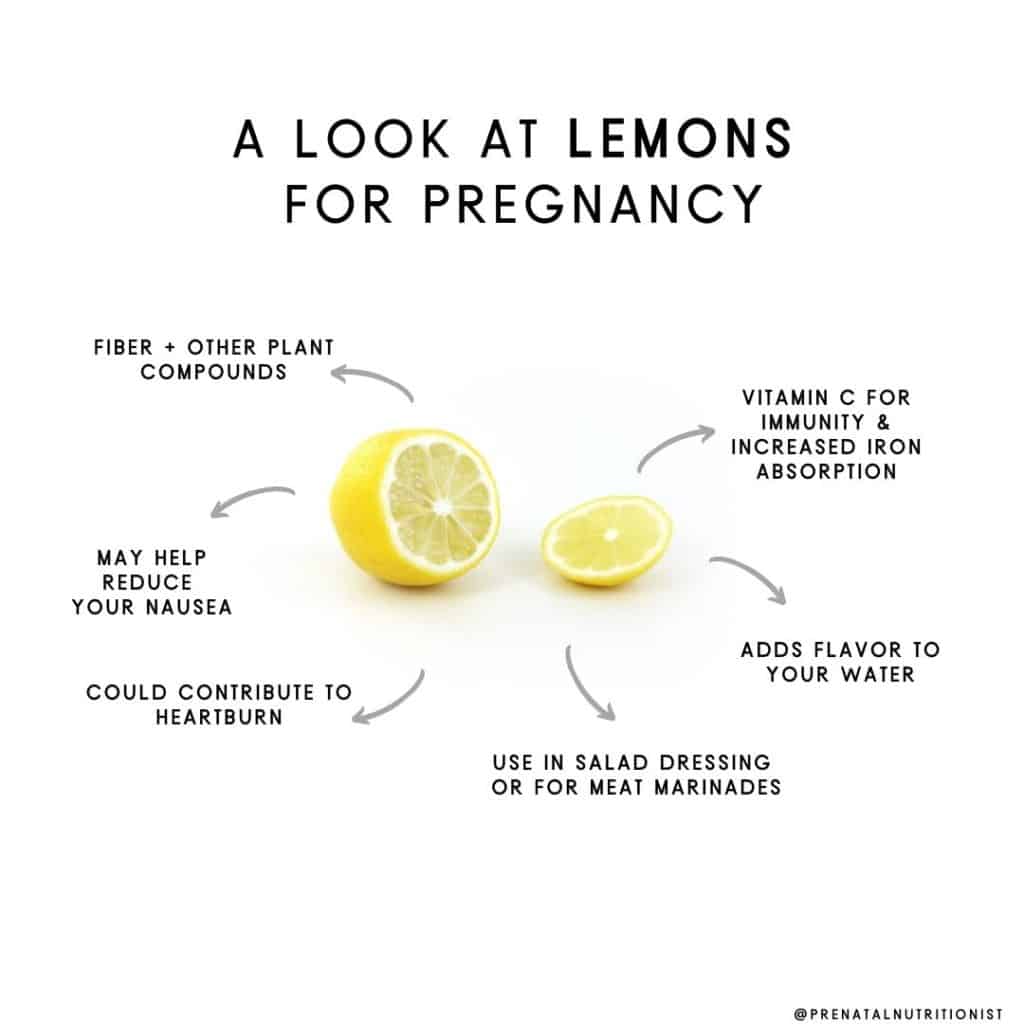
Vitamin C, immunity, and fetal development
Vitamin C is an important antioxidant and helps build immunity in the body. During pregnancy, women are at higher risk of developing illnesses because your body is protecting both you and baby. Keeping your immunity up during this time is critical.
Not only is vitamin C important for mom’s immunity, but it has also been linked to birth weight and length (2). Especially when both vitamin C and E were high in the second trimester of pregnancy, according to this study.
Another study also found that an increased intake of vitamin C in mid-pregnancy resulted in increased fetal growth and infant growth for up to 6 months of age (3).
Lastly, vitamin C increases the absorption of iron, another crucial nutrient for a healthy pregnancy. Squeezing lemon on high iron foods will increase the absorption, ideal for those who struggle with anemia or are only getting their iron from plant foods (4).
Does lemon help with nausea?
“Morning sickness” or nausea can be tough especially in the first trimester.
Some research suggests that diffusing lemon essential oil may be a great homeopathic remedy to help settle your stomach.
In 2015, 100 women were studied who complained of mild to moderate nausea with or without vomiting (5).
In this double-blinded study, half were given lemon oil to inhale when they felt nauseous and the other half were given a placebo. At least 25% of women who used the lemon essential oil found it to be effective in preventing nausea and vomiting (5).
A few drops in your diffuser may be a great homeopathic remedy to try.
Keep in mind, ingesting essential oil of any kind is not recommended as they are not regulated by the FDA.
Lastly, be careful when using lemon drops for nausea as these usually contain a lot of sugar.
Lemon juice in pregnancy, is this safe?
If you’re craving a tall glass of lemon juice, there may be a few reasons to put on the brakes.
Sugar
The concern with many fruit juices is the sugar content and lack of fiber.
Although the sugar is more natural, coming from a fruit, it is likely you are getting much more by drinking the juice compared to eating the actual fruit. You are also missing out on important fiber when you juice fruits as opposed to eating them.
Heartburn
Lemon juice is acidic in nature and can be a bad recipe for heartburn. Even drinking beverages like lemonade can contribute to heartburn which is already a common annoyance during pregnancy.
Tooth erosion
Tooth erosion means losing the enamel coating that covers your teeth and is not a good thing.
Pregnant women are already more susceptible to inflammation in the mouth and potentially other tooth issues. A 2015 study showed lemon juice to be one of the top beverages contributing to tooth erosion, even higher than the soda Coca-Cola (6).
Is lemon water good for pregnancy?
Hydration during every stage of life is important, and pregnancy is no exception.
Water helps carry nutrients and oxygen to our cells, regulates body temperature, and helps the kidneys to excrete toxins (7).
Women who are pregnant should increase their water intake as their body weight and blood volume is constantly changing.
More fluid sounds like a nightmare to most pregnant women but can also aid in relieving constipation and help to prevent urinary tract infections (8).
Adding lemon to your water is more than safe in pregnancy and can help add some zest and flavor to increase your intake when plain water sounds unappealing.
How else can I use lemon in pregnancy?
- In salad dressing
- Wedges in water
- Lemon juice in meat marinades
- Lemon oil in a diffuser
- Baked goods
- Garnish with the rind zest
The Bottom Line
- All in all, lemons during pregnancy are perfectly safe for you and your baby.
- The vitamin C in lemons contributes to increased immunity, adequate fetal growth, and enhanced iron absorption.
- They may also be the holistic remedy you are looking for to relieve that dreaded nausea or the perfect way to zest up your water.
By Lauren Gannon, RD and Ryann Kipping, MPH, RDN, CLEC | Owner & Founder
Dates
Coconut
Chia Seeds
Have you been wondering if eating chia seeds while pregnant is beneficial to you and your baby?
Chia seeds come from a desert plant, from the mint family, called Salvia hispanica. You may know them for their dark, black color, and all of the fun recipes that chia can be incorporated into (chia pudding, anyone?).
While pregnant, you’re doing everything you can to make the healthiest choices possible for you and your growing baby. Let’s sort out the facts about chia seeds and pregnancy!
Are chia seeds safe during pregnancy?
Chia seeds are safe to eat during pregnancy and, like many other whole grains and seeds, contain numerous beneficial nutrients for pregnancy, which will be discussed more below.
What food group are chia seeds in?
Chia seeds are unprocessed, whole grains, and are the seed of the flowering plant Salvia hispanica grown in several Latin American countries, as well as Australia. Legend has it that ancient warriors attributed their strength and stamina to this tiny seed (1).
Chia seeds are either white or black in color, but you may be used to seeing the dark chia seeds in your local grocery store. There is no nutritional difference depending on the color of the chia seed, unless it is brown, which means it is not ripe.
They are 9% water, 46% carbohydrate (mostly fiber), 34% fat, and 19% protein (2).
These little seeds pack a plentiful nutrition punch. They are considered to be a complete protein source, which means chia seeds contain all nine essential amino acids (3).
Amino acids are the building blocks for protein, and essential amino acids are so important to obtain from your diet because your body cannot make them.
Protein is important during pregnancy as it helps your baby grow (4). Protein needs vary person to person and your needs continue to increase as you move throughout pregnancy (5).
A woman who weighs around 150 pounds, needs close to 80 grams of protein per day in early pregnancy.
Nutrient breakdown
1 Tablespoon (13 grams) Chia Seeds
Energy: 60 calories
Carbohydrates: 5 g
Fat: 4 g
Protein: 2 g
Fiber: 4 g
Calcium: 80 mg
Iron: 1.08 mg
Cholesterol: 0 g
All values provided by the USDA nutrient database
Benefits of chia seeds during pregnancy
Omega-3 fatty acids
Chia seeds are an excellent source of omega-3 fatty acids, containing 7 grams per 1 tablespoon.
Most of the omega-3 fatty acids in chia seeds are ALA (alpha-linolenic acid), which exerts antioxidant and anti-inflammatory effects (6).
ALA is a type of omega-3 fatty acid, just like DHA, however, they are not equivalent in function.
DHA is a crucial nutrient in the development of your baby’s brain and has been studied quite a bit in relation to cognition after birth (7).
ALA is converted to DHA but at a very poor rate. Therefore, you still need to get DHA in your diet from sources that contain DHA directly, like fish (8).
Most experts agree DHA is the most important omega-3 and we know this is true during pregnancy. But, not to worry, chia seeds have other benefits besides containing high amounts of ALA.
Fiber
Chia seeds contain a unique blend of soluble and insoluble fiber, so they can be beneficial in alleviating pesky gastrointestinal (GI) issues, like constipation.
The high fiber content coupled with protein may even help reduce your risk of developing gestational diabetes (9). With guidance from your dietitian or doctor, chia seeds may also make a great diet addition if you have been diagnosed with gestational diabetes (2).
One study suggests chia seeds can help mitigate the adverse effects a high sugar diet has on our health from during pregnancy to adulthood (10).
Mineral content
Lastly, chia seeds are high in a variety of minerals important for pregnancy such as iron, calcium, magnesium, zinc, and phosphorus.
They also provide a wide variety of antioxidants (2).
Interestingly, chia flour has been shown to increase hemoglobin concentrations in animals (11). Swapping wheat flour for chia flour also increases the fiber content of the product (12).
If you are looking to get creative in the kitchen while also increasing your iron levels, this may be your new favorite ingredient!
Are there risks to eating chia seeds during pregnancy?
Chia seeds are a low-risk food to consume in and outside of pregnancy, but there is one important note to mention.
Some people report GI discomfort when overindulging in chia seeds such as constipation, diarrhea, or general discomfort like bloating. If you do notice any of these symptoms, you can try soaking them prior to consuming them.
Before adding more chia seeds to your diet, consult with your registered dietitian or doctor, especially if you are on any medication.
Next, we will discuss the appropriate portion sizes.
How many should I eat?
Adding 1-2 tablespoons of chia seeds to your diet is a good start. It’s important to increase your water intake due to the fiber content discussed above, however, you do not need to soak them in water or ground them before consuming unless you have a GI condition that warrants this.
If you enjoy chia seeds and tolerate them well, you can add more than the initial 1 tablespoon to your diet a day, but like anything else, moderation is key.
Research shows that eating high amounts of ALA has no adverse effects on pregnant women consuming up to 600 mg of ALA per day (13).
Although keep in mind what we discussed above, you should not be relying on chia seeds for your daily dose of omega-3’s.
How to include chia seeds in your prenatal diet
Chia seeds can virtually be thrown on any food or dish. Even the more involved recipes that use chia seeds are easy and fun to make.
Here are several ways to include chia seeds in your diet:
- Use as a yogurt topping
- Add to smoothies
- Add to oatmeal
- Make chia pudding
- Add to overnight oats
- Add to avocado toast
- Swap regular flour for chia flour
- Have you heard of chia water?
Mix ¼ cup of chia seeds in 4 cups of water. Let it sit for 20-30 minutes, then enjoy. Additionally, you can add some chopped fruit to give it a flavorful addition.
The Bottom Line
- While there isn’t a lot of research on chia seeds while pregnant, the general consensus is that consuming chia seeds during pregnancy is safe, and even beneficial to a growing baby.
- Chia seeds do contain omega-3’s but even better is their high fiber and mineral content.
- Adding them to your diet may even help balance your blood sugars and decrease your chance of developing gestational diabetes.
- If you want to start adding them to your prenatal diet, there are many recipes you can try such as chia pudding or simply adding them to your smoothie.
- It may take some time to get used to the flavor and texture of chia seeds, but it’s well worth it for all of the powerful benefits these tiny seeds provide.
By Alexa D’ Orazio, MS, RDN and Ryann Kipping, MPH, RDN, CLEC | Owner & Founder
Preconception Testing
Preconception Checklist
Soy
Food Safety
Avoid List
Caffeine
Zinc
Soft Cheeses
Selenium
Potassium
Manganese
Magnesium
Iron
Constipation
Fatigue
Headaches

Why do some people get headaches during pregnancy?
Some people may be more prone to headaches during pregnancy than others, usually those who experience headaches or migraines frequently outside of pregnancy (1). Even outside of pregnancy, hormones play a big role in the development of migraines.
Headaches are usually more prevalent in the first and second trimesters. Most headaches during pregnancy are tension headaches, but could also be clusters or migraines. Some women who experience migraines outside of pregnancy notice a reduction in them during pregnancy– one study found up to 85% of people actually notice remission of migraines during pregnancy (but if you’re not part of this group that goes into remission during pregnancy, we cover migraines more below) (2).
Hormonal shifts, weight gain, and higher blood volume may all be contributors to headaches during pregnancy (1). Headaches in the later stages of pregnancy may be a sign of high blood pressure and should therefore be considered a red flag to mention to your doctor (3).
The good news is that there are many modifiable factors that you can do to help reduce your risk of developing headaches, their overall severity and frequency, and their management of them during pregnancy.
How can hydration levels impact headaches?
This might seem obvious, but sometimes we need constant reminders of how important water is, especially if you are prone to headaches. One hundred ounces of fluids per day is a good goal, which includes all fluids, not just water.
However, only drinking lots of plain water isn’t always enough to fully hydrate your cells, which means you could be drinking all the water in the world, but your cells aren’t actually absorbing it, so you continue to be dehydrated.
What is cell hydration, and why is it significant for overall hydration in the body? Let’s discuss it!
What is cellular hydration, and how can I boost it?
Feel like you’re always chugging water but never satisfied? Always thirsty and feeling like it goes right through you?
These are signs your cells aren’t actually absorbing the water you’re taking. You need to boost your cellular hydration by drinking water with minerals! Minerals, which also function as electrolytes, are vital to ensuring proper hydration on a cellular level because they help cells attract water (4).
Here are some ways you can boost your cellular hydration:
- Get minerals in both your food and drinks: Enhance your cellular hydration with sodium by simply adding a dash of unrefined salt to your water, and increase your intake of mineral-rich foods: fatty fish and dairy (calcium), leafy greens, nuts and seeds, and avocados (magnesium), cured and smoked meats, pickles, and olives (sodium), and unsweetened coconut water, dried fruit, potatoes, and greens (potassium)
- Eat fruits and vegetables high in water content with small amounts of other nutrients as well, such as watermelon, bell peppers, zucchini, oranges, and cucumbers.
- Monitor your individual symptoms of dehydration rather than count the number of glasses you drink daily. Besides headaches, these include fatigue, brain fog, irritability, muscle cramps, dark urine, and dry skin. (Read more about fluids here.)
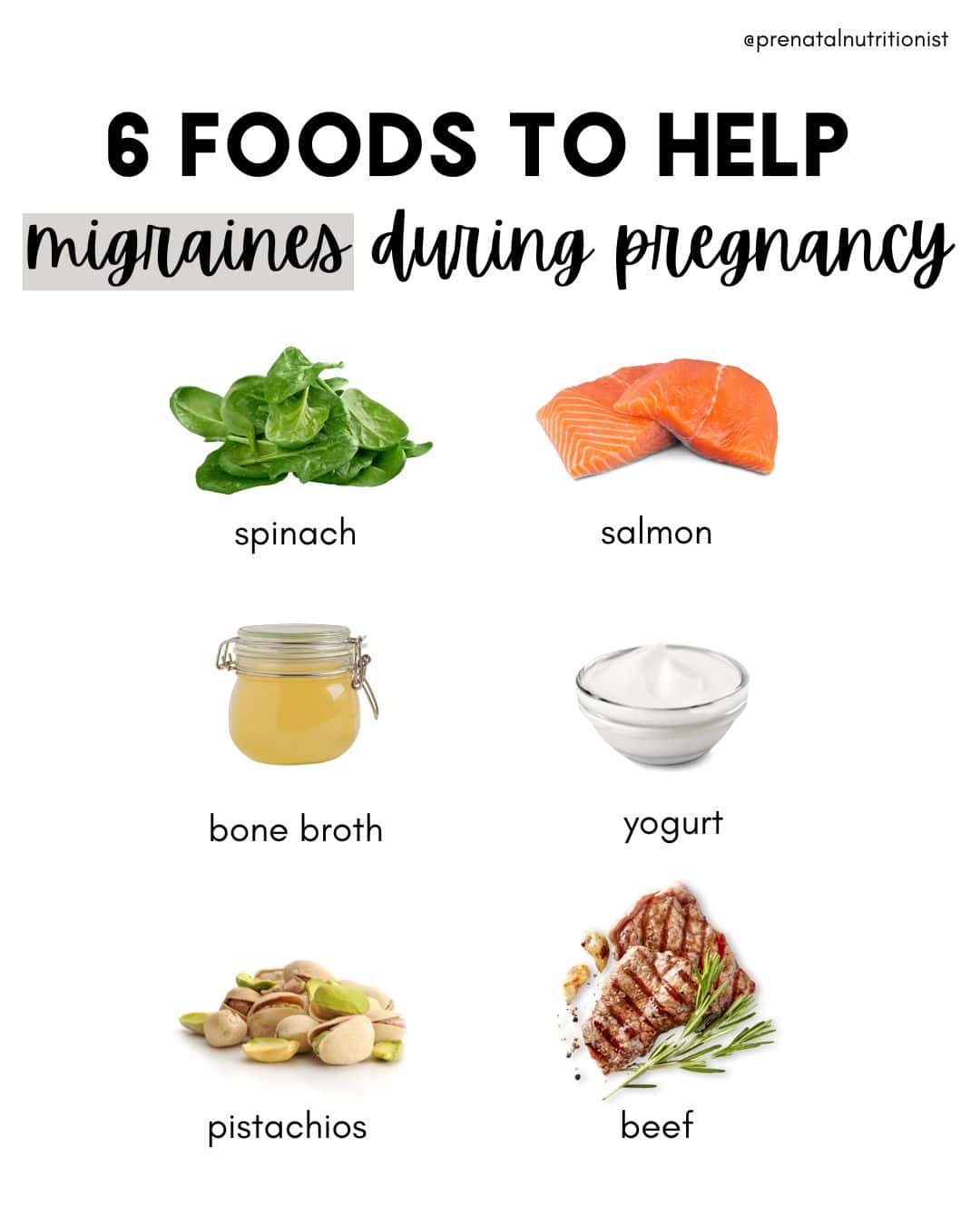
 What nutrients can help with headaches?
What nutrients can help with headaches?
Magnesium
Magnesium has been found to reduce the incidence and severity of tension and cluster headaches, and most people aren’t getting enough of it (5).
Increase magnesium-containing foods and consider a magnesium supplement. Start with 100 mg of magnesium glycinate (if constipation isn’t an issue!) and gradually increase this dose if need be. Check out the magnesium note for supplement recommendations.
Foods rich in magnesium to increase your intake include nuts and seeds, cooked spinach, and beans.
Vitamin B12
Increase vitamin B12-containing foods and consider extra B12 supplementation. Some research suggests vitamin B12 needs during pregnancy are 3 times higher than we once thought. Make sure your prenatal contains methylcobalamin.
Foods highest in B12 to eat daily are beef liver, clams, salmon and tuna, beef, and dairy. (Remember: this vitamin is only found in animal foods, especially meats and fish, which is another reason why avoiding these during pregnancy is problematic. Read more here)
Omega-3’s
Many people aren’t getting enough omega-3s, which is important to note for both pregnancy in general and headache and migraine prevention. Some studies have found omega-3’s can be helpful in preventing these, likely due to their anti-inflammatory role, which we know is a common driving factor in migraine development (6, 7, 8, 9).
If you’re looking for ways to get in more omega-3s for both your and your baby’s brain, increase your intake of fatty fish (2-3 servings per week) or take high-quality fish oil (see recommendations here).
Probiotics
Not only are probiotics important for cultivating gut health for pregnancy in general (especially since you’ll pass your gut to your baby), but by supporting gut health which impacts brain health through the gut-brain axis, probiotics have also been found to be a helpful food for headache and migraine prevention!
One study (in children) found that using probiotic supplements seems to significantly affect the severity and frequency of migraine headaches compared to the placebo, and daily consumption of painkillers was significantly reduced in the probiotic group compared to the placebo group (10).
Many other studies have found similar results for probiotics reducing the frequency and intensity of attacks (11, 12, 13, 14).
Increasing your probiotic consumption through foods is the most ideal, especially if you’re consuming fermented foods like sauerkraut, kimchi, and miso at least 3 or more times weekly. Greek yogurt is another good source of probiotics.
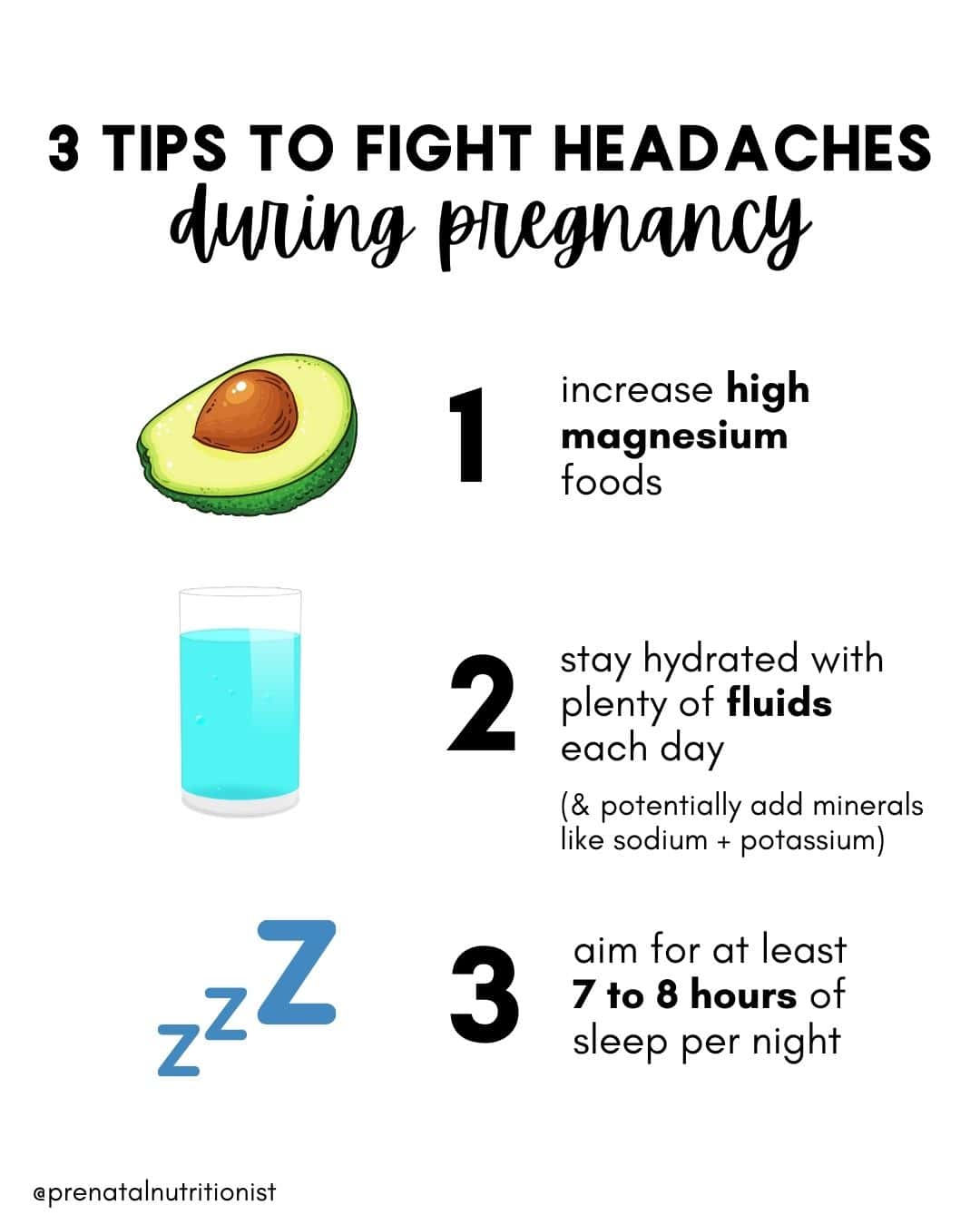
Can sleep help with headaches?
Ensuring appropriate sleep is important, and lack of it may contribute to increased headaches (15). Aim for at least 7-8 hours per night and consult with a physical therapist if you need help determining appropriate sleep positions.
Getting enough quality sleep can be easier said than done during pregnancy-here are some tips to help you cultivate better sleep during this time:
- Create intentional wind-down time with a 20-minute (or more) bedtime routine. This routine can be a mix of the usual bedtime hygiene tasks (PJs, skincare, brushing teeth) as well as at least one more relaxing activity you enjoy to help you wind down: reading, journaling, an artistic activity, knitting/crocheting, prayer, or even a game with your spouse
- Sleep with your phone as far out of reach as possible (and resist the urge to check it in the middle of the night!)
- Make your sleep space conducive to good sleep: as dark and as cool as possible to reduce wakefulness and support better sleep quality (16)
- Drink a calming pregnancy-safe tea or one, especially for sleep support, such as a chamomile blend or Needed’s sleep + relaxation support.
Can exercise help with headaches?
Partaking in some form of exercise for 30 minutes 3 times per week has been shown to reduce the occurrence of headaches (keep in mind the national recommendation for exercise, in general, is 150 minutes per week, which means getting in 30 minutes at least 5 days per week) (17, 18).
Exercise doesn’t have to be intense to be effective, and ideally, it should always be a form of movement you enjoy! Walking, dance, a prenatal exercise class online or on an app…anything to support increased blood flow.
 Can eating certain foods trigger headaches and migraines?
Can eating certain foods trigger headaches and migraines?
While the exact causes of migraines are sometimes hard to pinpoint, for about 25% of people with migraines, certain foods can be identified as a contributing factor (19).
One possible reason could be that immune-mediated food sensitivities may be involved, as IgG antibodies can be a cause of inflammation (20). Identifying food triggers for some can be key for some in managing migraines; one study found that eliminating foods that led to these IgG reactions controlled migraines without the need for medication, while another found eliminating foods that led to IgG antibodies led to a significant reduction in the number of migraines or migraine-like headaches at four weeks (21, 22).
If you notice certain foods trigger headaches and migraines for you before pregnancy, these may be the same or different than they were before pregnancy.
Common triggers include (23):
- Caffeine (and caffeine-containing foods such as chocolate or teas)
- Artificial sweeteners
- Glutamic acid in MSG
- Foods high in tyramine: aged cheese, cured meats, pickled or fermented foods
- High-lactose dairy products
As you might notice, some of these foods are beneficial for pregnancy, so if you notice any correlation between a reduced tolerance of any of these and increased headache incidence (such as high lactose dairy and probiotic foods such as fermented foods), make sure you are replacing these with other food options that contain the same nutrients to ensure you are not missing these in your diet during this time.
If you suspect a food or food group could be triggering migraines, it’s recommended that you work with a licensed nutrition professional, as it’s not recommended that you self-diagnose food sensitivities and/or eliminate any whole foods (non-processed foods) during pregnancy.
Can I take medications to help me deal with headaches?
Consult with your physician before taking any medication during pregnancy. Usually, options during the first trimester are limited, but you may be able to take a pain reliever in the later stages of pregnancy. You can also check the Mother to Baby database.
In general, NSAIDs are discouraged, especially after 20 weeks of pregnancy, along with Ibuprofen and naproxen, but Tylenol is considered a safer medication to take during pregnancy (24).
You can also try alternative ways to deal with pain if you’re able, which are covered more at the end of this note.
What should I do if I’m dealing with migraines?
Migraines are complex issues, so if you’re dealing with this intensity level of headaches, it’s ideal to work with a functional practitioner who can help you investigate possible root causes of these. An estimated 10% of women deal with migraines during pregnancy (25).
Similar to regular headaches, migraines can be caused by rising estrogen levels during pregnancy, and though they can present for the first time during pregnancy without being tied to a specific condition (like preeclampsia), it’s always a good idea to mention them to your doctor (26).
Migraines can often be attributed to genetic, environmental, and lifestyle factors. While we don’t know exactly what causes migraines (especially as there are multiple possible contributors for each person), common triggers include:
- An overall pro-inflammatory and oxidative state (27)
- Insulin resistance (28)
- Inflammatory diseases (hint: nearly all diseases and conditions have inflammation as at least one partial root contributing factor (29)
- Mitochondrial dysfunction (30, 31)
- Stress, environmental allergens, and food allergies or sensitivities (32)
- Comorbid pain conditions
- Poor sleep
The good news is that aside from genetic factors, many factors can be modified by addressing these diet and lifestyle factors!
Nutrients and nutrition for migraines
Did you know there are specific nutrients that have been found to help support mitochondrial function and reduce the chances of recurring migraines?!
Nutrients that have been found to help prevent migraines include folate, riboflavin, coenzyme Q10, and magnesium (32).
It makes sense since folate can help with migraines because it is involved in DNA methylation, and research has found a folate-rich diet (one that is recommended anyway during pregnancy) can be an area to target migraine management and relief (33).
Studies have found that people with migraines often have increased levels of oxidative stress and pro-inflammatory cytokines, which riboflavin can help reduce, in addition to reducing migraine incidence overall (34).
Coenzyme Q10, aka CoQ10, has been found in studies to reduce migraine incidence, severity, and duration (35). Check out supplement recommendations in the CoQ10 note.
Magnesium is an important nutrient to focus on for headache and migraine prevention as well since studies have found at least 50% of people who get them are deficient in magnesium (36, 37). Being deficient in magnesium has been found to significantly contribute to the development of migraines (38).
So if you frequently get migraines, getting your magnesium levels checked and increasing your magnesium intake through food (and possibly a supplement if your levels are low) is a good idea!
A lower-carb diet for migraines
In addition to the nutrients above, a way of eating that has been specifically linked to helping manage many different neurological conditions, including migraines, is the ketogenic diet or a lower-carb diet (yes, it is safe during pregnancy– see our carbs note if you have concerns).
Because a low-carb diet supports cell processes in the brain and metabolism, along with mitochondria function, balanced serotonin levels, and neuroinflammation (39, 40).
Another reason a low to very low carbohydrate diet approach may be helpful for reducing migraines is that this is an effective way to manage blood sugar (41). Increasing evidence suggests that migraines may be the result of an impaired brain glucose metabolism, as well as dysfunctional mitochondria in the brain (42).
This could also be because peripheral insulin resistance has been thought to extend to the brain, leading to insulin resistance in the brain, and insulin resistance, in addition to metabolic syndrome, is more common in people with migraines (43, 44). (Just another reason why managing blood sugar matters for your overall health and helping you feel your best!)
If you are interested in implementing a distinctly low-carb diet during pregnancy, it’s highly recommended that you work with a licensed nutritionist or dietitian who can guide you in following one in a healthy way during pregnancy so you can ensure all your nutrient needs are met.
 What are other interventions that can help me manage headaches and migraines?
What are other interventions that can help me manage headaches and migraines?
Besides using a provider-approved pain reliever, here are some interventions you can try if you are looking for other alternatives, either instead of or in addition to pain-relieving meds:
- A headache cap
- Chiropractic care
- Massage therapy
- Acupuncture
- Addressing areas of stress and overall mental health
- Essential oils (do not ingest) like an aromatherapy stick for headaches and migraines (this one or this one)
- Stretching
- Extra rest
- Avoiding bright screens at night and wearing blue light glasses to limit eye strain (as this can trigger headaches)
- Drinking a soothing tea like this one (make sure you check the ingredients of any “headache tea” first, many include teas in blends that should be avoided during pregnancy)
When is a headache or migraine of concern during pregnancy?
Always mention headaches to your physician, especially if you have a family history of migraines, high blood pressure, seizures, or diabetes (45).
New or refractory headaches, hypertension, and abnormal neurological signs are important “red flags” to consider in particular (46). The Bottom Line
The Bottom Line
- A number of factors, like hormonal shifts, weight gain, and higher blood volume, could cause headaches during pregnancy.
- Aim for 100 ounces of total fluids per day with at least one glass per day with added salt or other sugar-free minerals to support cellular hydration.
- Eat foods high in magnesium, vitamin B12, omega 3s, and probiotics.
- Ensure you’re getting adequate sleep and physical activity every day, at least 7 hours of sleep each night, and 30 minutes of movement most days.
- If you’re dealing with migraines, make sure you’re getting enough riboflavin, coenzyme Q10, folate, and magnesium. Consider an additional magnesium or CoQ10 supplement.
- Consider lowering your carb intake. A low-carb diet has been found to be helpful for minimizing migraines, as well as addressing possible root factors, including inflammation, insulin resistance, mitochondrial dysfunction, stress, environmental allergens, food allergies or sensitivities, comorbid pain conditions, and poor sleep. Working with a functional practitioner to address these root causes is ideal.
- Review approved medication and/or other remedies to help with pain management, such as aromatherapy, chiropractic care, a headache cap, and drinking pregnancy-safe tea with your provider.
Written by: Ryann Kipping, MPH, RDN, LDN, and Claire Gilmore, MSCN, CNS, LDN
Leg Cramps
Pica
Swelling
Vegetarian
Dairy-Free
Fish-Free
Egg-Free
Nut-Free
Vitamin B12,Cobalamin
Weight Gain in Pregnancy
Vitamin B7,Biotin

What is biotin?
Biotin is a water-soluble* vitamin also known as B7 (1).
You may have heard of it as a supplement to keep your hair, nails, and skin healthy. Tread carefully around biotin supplements advertised as reducing hair loss, acne, or eczema as there is no research to support this (2).
It is still in the early days of biotin research and scientists are still figuring out B7’s role in the body. New studies are examining its function during pregnancy (3) (4) (5) (6) (7).
*This means the vitamin dissolves in water, so any excess biotin you consume that your body does not need, will simply get urinated out.
What is biotin’s role and why is it important during pregnancy?
Biotin is necessary for forming fatty acids and glucose, which are used as fuel by the body (8).
B7 vitamin is also essential for maintaining metabolic processes. For example, synthesizing amino acids from the protein you consume (1) (9).
Biotin has recently been shown to play a role in fetal growth and development (4) (5) (10).
Research is still being done into the transplacental transport of biotin from mother to fetus, but in animal studies, biotin deficiency has shown adverse effects on fetal growth, causing malformations such as cleft palate (6) (11).
What are the signs of deficiency and potential consequences?
Mild deficiency is unlikely to be highlighted on bloodwork and you may not feel any different from usual (9) (11).
Severe deficiency may show itself as hair loss or red scaly rashes. High blood levels of cholesterol have also been linked to biotin deficiency (3) (12).
Approximately 50% of pregnant women are biotin deficient (2) (7).
Animal research studies are showing evidence of biotin deficiency impairing fetal growth (11). Some studies state the risk in humans is low/non-existent (3) but the exact role of biotin during pregnancy is still being researched so it is important to maintain adequate amounts throughout pregnancy and lactation. Biotin recommendations are discussed later.
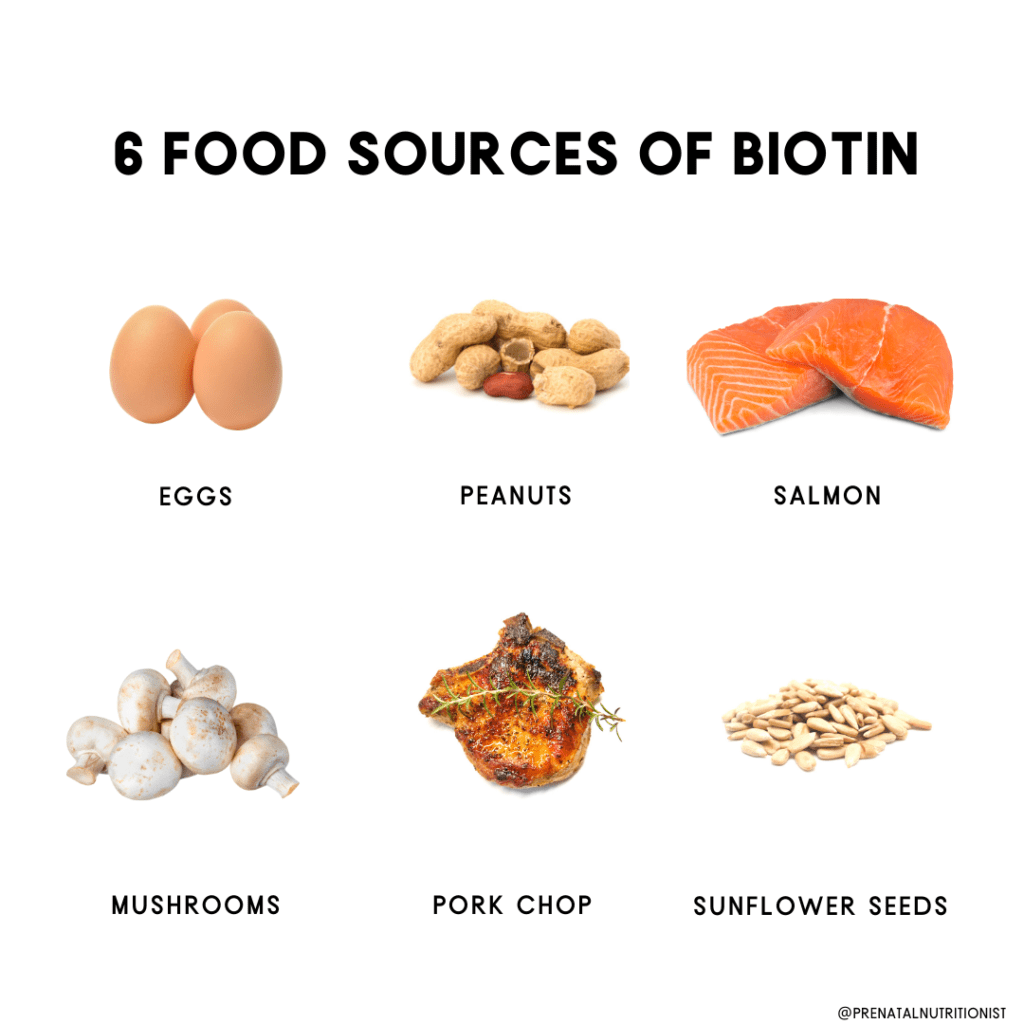
Where can I find biotin?
Our bodies cannot make biotin themselves, so we rely on our diet to provide adequate amounts of biotin (1).
Similarly, a fetus is completely reliant on the mothers’ diet for its biotin supply, which is transported via the placenta (9) (10).
Many foods contain higher levels of biotin when they are raw (13) but these should only be consumed raw if it is safe to do so, of course.
In contrast, the biotin available in eggs is best obtained when cooked – in raw egg whites, there is a glycoprotein that binds to dietary biotin meaning it cannot be absorbed. Cooking will prevent this binding from happening (8) (13).
Where can I find biotin?
Our bodies cannot make biotin themselves, so we rely on our diet to provide adequate amounts of biotin (1).
Similarly, a fetus is completely reliant on the mothers’ diet for its biotin supply, which is transported via the placenta (9) (10).
Many foods contain higher levels of biotin when they are raw (13) but these should only be consumed raw if it is safe to do so, of course.
In contrast, the biotin available in eggs is best obtained when cooked – in raw egg whites, there is a glycoprotein that binds to dietary biotin meaning it cannot be absorbed. Cooking will prevent this binding from happening (8) (13).
Below are the foods highest in biotin:
Micrograms (mcg) per serving
- Beef liver (cooked) 30.8
- Egg (cooked) 10.0
- Peanuts (roasted, salted) 4.91
- Egg yolk (cooked) 4.08
- Salmon (pink, canned in water) 3.69
- Porkchop (cooked) 3.57
- Mushrooms (canned) 2.59
- Sunflower seeds (roasted, salted) 2.42
- Hotdog, chicken, and pork (cooked) 2.06
- Strawberries (fresh) 1.67
- Hamburger patty (cooked) 1.65
- Almonds (roasted, salted) 1.32
- Sweet potato (cooked) 1.16
- Broccoli (fresh) 1.07
Amounts adapted from Staggs et al 2004
It is worth noting that most meats and cereals have been found to contain more protein-bound biotin than free biotin (9) (13).
Protein-bound biotin must be broken down before it can be used (1) (11). Free biotin is used to maintain all processes mentioned earlier (e.g. amino acid metabolism) and due to its water solubility, almost 100% is absorbed (9) (11).
Free biotin can be found in fresh fruit and vegetables, as well as supplements.
 How much biotin do I need before, during, and after pregnancy?
How much biotin do I need before, during, and after pregnancy?
There are three different ways of expressing the amount of any nutrient or vitamin (9):
EAR – Estimated Average Requirement
This is the minimum intake required to maintain a healthy level in the body.
RDA – Recommended Dietary Allowances
This is the amount of intake required to meet the needs of most healthy people.
AI – Adequate Intakes
This is only ever provided if there is not sufficient scientific knowledge to provide EARs or RDAs (3). These are based on experiments or observations of healthy people and represent a goal intake, like RDAs.
According to the European Food Safety Authority (EFSA), the AI of biotin is:
40 mcg for adults and pregnant women
45 mcg for lactating women
However, the research found that women with an average intake of 57 mcg still show signs of deficiency (4) and that approximately 2-3 times more than the current AI is needed during pregnancy and lactation (4).
More research into biotin is needed, but we know that toxicity does not occur as excess biotin is peed out (8).
So, it is safe to be taking supplements that contain around 100 mcg of biotin.
Adequate intake of biotin throughout early and late pregnancy, as well as post-partum, is important for mother and baby’s health (5).
Is vitamin B7 important for postpartum and breastfeeding?
As mentioned above, biotin is involved in energy metabolism, which is essential for daily activities, postpartum recovery, and breastfeeding.
Biotin is frequently used in supplements to support skin, hair, and nail health. Hair loss is a common postpartum concern (12). Unfortunately, no substantial evidence supports using biotin supplementation for hair loss (13, 14). Learn more about postpartum hair loss and what nutrition strategies may help here (LINK NOTE).
How much do I need postpartum?
There is no Recommended Dietary Allowance (RDA) set for biotin. An “Adequate Intake” (AI) has been established. The AI is the level assumed to ensure nutritional adequacy but is used when there’s not enough evidence to establish an RDA (15).
The AI for biotin is 30 mcg per day for women and 35 mcg per day during lactation. The Food and Nutrition Board (FNB) reports that the AIs they created are based on the amount of biotin in human breast milk consumed by infants and then using body weight to calculate AIs for other population groups (15).
Some research suggests that biotin intake above the current AI recommendation is necessary to meet increased demands during lactation (16).
Should I be supplementing?
Biotin can be found in some prenatal and pregnancy vitamins but not all of them, so it is worth checking.
The biotin in supplements is free biotin so your body and baby can absorb as much as needed.
As some research shows biotin needs are much higher during pregnancy and lactation (4) (5) (7), it may be necessary to supplement with biotin to meet your body’s needs. It is important to tell your health professional you will be doing this as it can affect various test results (14).
 Higher rates of biotin deficiency can be found in women with Irritable Bowel Syndrome (IBS) and Gastritis Disease (9), so if you have either of these or are undergoing anticonvulsant therapy*, check with your health professional about biotin supplementation.
Higher rates of biotin deficiency can be found in women with Irritable Bowel Syndrome (IBS) and Gastritis Disease (9), so if you have either of these or are undergoing anticonvulsant therapy*, check with your health professional about biotin supplementation.
*Anticonvulsant drugs can reduce your levels of biotin, but supplementation is effective if they are taken a few hours apart (9).
The Bottom Line
- Biotin is an essential nutrient for you and your baby.
- Incorporating fresh foods that are rich in biotin can reduce your risk of deficiency.
- Check your prenatal supplements to see if biotin is included.
- Continue with an increased level of biotin intake while breastfeeding.
Written by: Anna Redding, BSc Nutrition
Reviewed/edited by: Ryann Kipping, MPH, RDN, CLEC, Owner/Founder
Vitamin K
Vitamin E
Vitamin D
Vitamin A
Probiotics
Fluids
Carbs
Fats
Protein
Artificial Sweeteners
Chocolate
Honey
Herbs: A brief overview
Ashwagandha

Ashwagandha is a popular Ayurvedic adaptogen that is thought to increase vitality and strength, and level out your mood with its de-stressing effects (1).
In fact, one study saw a reduction in morning cortisol levels of healthy adults who took ashwagandha daily (1).
Cortisol is the pesky hormone that is released when you’re stressed, and too much can cause things like weight gain, and disrupt your sleep.
So, could ashwagandha be the answer to mood-balancing, stress-free days? And is it even safe to take during pregnancy? Let’s find out.
What is ashwagandha?
Ashwagandha is an evergreen shrub, Withania somnifera, that grows in India, the Middle East, and Africa. It is also called “Indian Winter Cherry” or “Indian Ginseng” and belongs to the nightshade family like eggplants.
Its root is said to smell like a horse and is available in powder form (2).
Ayurveda is a system of natural medicine that originated in India thousands of years ago. It’s believed that bodily imbalances and stress are the cause of disease, and Ayurveda incorporates certain lifestyle interventions and natural therapies to help you re-balance.
Is ashwagandha safe during pregnancy?
In a study done with pregnant rats, researchers observed no toxicity effect on the mother or the developing fetus at levels up to 2000 mg/kg/day (3).
If you have come across certain “mommy blogs” talking about the positive effects of ashwagandha during pregnancy, tread lightly. These mother-to-mother support systems are helpful in some ways, but should not be taken as the word when it comes to YOUR pregnancy.
When it comes to the safety of herbs and other natural remedies, it is best to speak with your doctor regarding your personal circumstances. Many medical professionals caution against taking ashwagandha while pregnant as it may induce a miscarriage at high doses (4, 5).
Those with thyroid imbalances should take extra precautions since ashwagandha may worsen symptoms (6).
While there isn’t much research on ashwagandha and pregnancy, there is some research done on the effects it has on stress, and even on cancer, in animal and human studies (7).
Nutrition breakdown
100 g Ashwagandha Powder
- Calories: 45 calories
- Carbohydrates: 10 g
- Sugar: 0 g
- Fat: 0 g
- Protein: 1 g
- Fiber: 0 g
- Potassium: 282 mg
- Calcium: 32 mg
- Iron: 0.31 mg
- Phosphorus: 20 mg
- Niacin: 0.4 mg
All values provided by USDA nutrient database.
Are there benefits to consuming ashwagandha while pregnant?
As mentioned earlier, there is not a lot of research on ashwagandha and pregnancy, but there are studies showing positive effects in rats and healthy humans (8, 9).
A few different articles reviewed the current literature published testing ashwagandha and its role in cancer prevention.
What they saw across these studies was that withanolides (naturally occurring compounds in ashwagandha that have been used for 3000 years in traditional Ayurvedic practice for its pharmacologic effects) can debilitate the inflammatory response and certain enzymes involved in the metastatic progression of cancer (10, 11).
The most popular and widely seen reason for supplementing with ashwagandha is for its stress-reducing properties.
In this study, healthy adults consumed 300 mg of ashwagandha powder in capsule form for 60 days, and the researchers saw a 27.9% reduction in cortisol levels on day 60 compared to day 0 (12)!
Stress (and having increased levels of cortisol circulating through your body) can increase your heart rate, make you prone to headaches or digestive problems, cause sleeplessness, and weight gain.
Can ashwagandha boost male fertility?
What’s interesting is that quite a few studies have been completed on ashwagandha for men.
A study completed in 2009 showed that men who took 5 mg/day of ashwagandha root powder for 3 months had less stress and improved semen quality (13).
Three other studies also showed significant improvements in male fertility with ashwagandha supplementation (14, 15, 16).
Are there potential side effects?
A literature review of 69 human studies reported no serious adverse effects of oral ashwagandha intake (17). There were some minor and mild effects, like abdominal discomfort and drowsiness, for these were minimal and did not last.
In addition to those findings, they also saw that no toxicity effects were present months after consuming this adaptogen.
However, keep in mind, these results were from non-pregnant individuals.
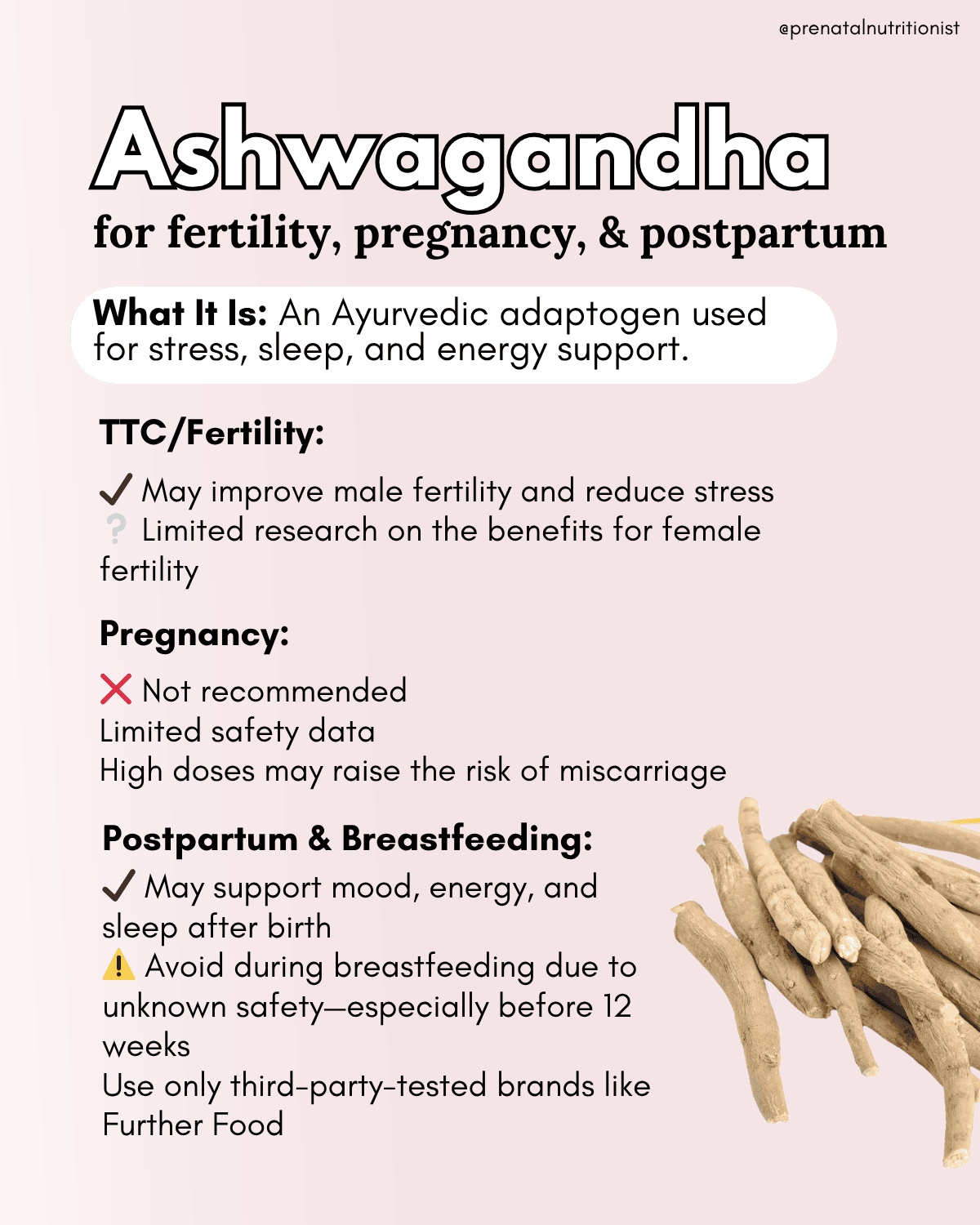
Is ashwagandha safe during postpartum and breastfeeding?
Studies in adults, not specific to postpartum, have found ashwagandha to be generally safe (18). Serious adverse side effects are overall rare (18, 22). This suggests that for a postpartum individual who is not breastfeeding, ashwagandha’s safety profile would likely be similar to that of the general adult population.
Traditionally, ashwagandha has been used postpartum worldwide in Ayurvedic medicine for its adaptogenic effects (19). It is thought to provide a sense of calm, boost energy levels, and help alleviate sleep disturbances.
Unfortunately, its consumption during breastfeeding is a gray area.
There is no data on the safety of taking ashwagandha during lactation and its level of transfer into breast milk (19). Larger health institutions, such as the National Institutes of Health (NIH), recommend avoiding it during breastfeeding due to a lack of data (18, 19, 21). Some herbalists and integrative practitioners consider it a safe herb for breastfeeding due to a lack of data pointing to contraindications or adverse effects during this time. Even so, some recommend waiting until the nursing infant is at least 12 weeks old.
Also, note that supplements can vary widely in quality. We always recommend sticking with third-party tested options. Further Food is a quality brand that offers premium ashwagandha (discount code: RYANN18).
Are there benefits to consuming ashwagandha during postpartum and breastfeeding?
Research in the general population suggests that ashwagandha may help reduce stress and anxiety and support improved sleep and energy levels (20). These potential benefits could all be helpful for postpartum, especially those experiencing stress and sleepless nights.
There is no specific research on ashwagandha for postpartum anxiety and depression. However, research in the general population has found that ashwagandha may help reduce mild to moderate symptoms of anxiety and depression (22, 23).
How can I use ashwagandha?
Ashwagandha is commonly blended into smoothies or other hot drinks to enjoy.
You can drink your adaptogenic beverage at any time of the day, though with the potential sleepy side effects mentioned earlier, you may want to try it at night.
Without altering the taste, you can even sprinkle it into the food you make, as long as you use less than a teaspoon of ashwagandha powder.
Alternatively, you (or your partner) can take it in capsule form while trying to conceive, if okayed by your physician.
The Bottom Line
- Since there are very few studies looking into ashwagandha while pregnant, you may want to wait to try out this trendy adaptogen until after your baby is born.
- Ashwagandha has been around and used for many years in Ayurvedic medicine, and could be a potentially positive herb to add to your daily routine.
- If you are interested in the anti-stress effects, know that there are many other ways to reduce stress, like exercising, meditation, talking and laughing with loved ones, or doing some of your favorite activities.
- There are some promising results for male fertility, but no significant results for female fertility, unfortunately.
- Ashwagandha may support stress, sleep, and energy during postpartum. Still, due to a lack of safety data and unclear transfer into breast milk, it’s generally not recommended during breastfeeding, especially before 12 weeks postpartum.
CBD Oil
Thyroid Nutrition
Elderberry
Anemia
Maca

You may have heard of maca recently, the hottest food trend for people on a fertility-boosting journey.
It’s touted to have a multitude of benefits, especially in the reproductive realm. But is maca safe during pregnancy or just another unproven trendy “health’ powder? We’ve got all the details on Maca during pregnancy below.
What is maca?
Maca is a native root plant from Peru. It is a cruciferous vegetable, like broccoli and cauliflower. It is often available in powder form, and many people report the taste as nutty.
There are three types of maca: red, yellow, and black. Different types of maca have different effects: black maca is more effective for men’s sperm production, motility, and semen volume (1).
If you read into the details of maca, it’s traditionally used to enhance fertility and is also said to improve energy and mood (2).
Most individuals who take maca powder blend it in their smoothies daily. However, other uses traditionally have included making it into teas and adding it to oatmeal, soups, and stews (3).
While there isn’t much research on maca during pregnancy, there is some research on maca and fertility. However, the amount of research done with maca, in general, is quite limited and typically uses animals or human males as research subjects or perimenopausal women.
Can Maca help you get pregnant?
Research for maca and fertility outcomes
Regarding women’s fertility, the research is scant and very inconclusive.
Many more studies and evidence support the use of maca for male fertility. Overall, maca has been found to improve semen parameters in men through increased sperm production and motility (3).
No studies have found it to have much effect on women’s hormones before menopause, and even fewer have studied it regarding pregnancy or conception.
Are there other benefits to consuming maca outside of pregnancy?
In minimal studies, maca was thought to potentially be able to support menopausal symptom treatment (4, 5). In one treatment, maca reduced the frequency and severity of individual menopausal symptoms, making it a natural alternative to Hormone Replacement Therapy (HRT) (6). In another study, maca reduced anxiety and depression in postmenopausal women (7).
Though these are not conclusive and research at this time is limited, maca does seem to have positive effects for those in the peri or postmenopausal stages for helping to manage symptoms at these stages.
Is maca safe during pregnancy?
The research needs to be more varied and plentiful.
In short, we don’t know. Since there is no sound scientific evidence or substantiated claim regarding maca consumption during pregnancy, most professionals do not recommend consuming maca or any other unregulated or unknown supplement (8).
We just don’t know if or how it could affect your baby.
Maca nutrition breakdown
1 Tablespoon Maca Powder (x):
- Calories: 30 calories
- Carbohydrates: 6 g
- Sugar: 4 g
- Fat: 0 g
- Protein: 1 g
- Fiber: 2 g
- Potassium: 130 mg
- Calcium: 20 mg
- Iron: 0.4 mg
Are there benefits to consuming maca while pregnant?
Maca is considered an adaptogen, meaning it helps your body adapt to stress. Adaptogens are trendy right now, so it makes sense maca is also part of this conversation.
While it’s fun and exciting, and possibly good for you to incorporate these adaptogens into your diet, again, there is little to no scientific research indicating that they’re safe for pregnant women.
The Botanical Safety Handbook sees “no identified problems for use during pregnancy or breastfeeding” for several adaptogens, including maca (9). However, a lack of evidence does not necessarily signify it is pregnancy safe.
 Are there potential side effects?
Are there potential side effects?
According to multiple research sources related to maca consumption, no adverse or toxic levels are reported in animal or human trials.
However, professionals still caution about the utilization and dosage since each individual can react differently.
As previously stated, there is no research on using maca during pregnancy or maca root while pregnant. The potential for adverse side effects or birth outcomes is unknown.
Since we know it can potentially affect hormones, it may be best to avoid it if you have or have had conditions related to hormone imbalances related to estrogens, such as endometriosis, breast cancer, or fibroids, or if any of these runs in your family. It may also be best to avoid maca if you have a thyroid condition (since this impacts your hormones), and talk to a professional knowledgeable about your history and herbs like maca if you want to use it.
Avoid maca if you are currently pregnant or breastfeeding.
If I include maca in my diet, which product should I buy?
If you would like to include maca in your diet while trying to conceive or during postpartum and beyond, here are a few recommendations while shopping for maca and which ones we recommend.
Gelatinized (also known as “activated maca” vs. raw maca: Gelatinisation is a cooking process that helps make maca safer to consume, giving us more potential health benefits from the maca.
While raw maca has some higher amounts of more bioavailable compounds (such as fatty acids and enzymes destroyed during heating), raw maca is much more susceptible to growing mold. It cannot be stored for long periods.
The mold that can grow on raw maca can adversely affect your gut and entire body, and is known to taste sweeter than raw maca. The safest form of maca is commercially called gelatinized or activated maca, which has gone through high-pressure steam to kill the mold and sanitize it.
Due to the removal of the starch, the activated maca powder contains nutrients that are better absorbed and more readily available. One study found that these nutrients were best absorbed in the cooked form in a study observing the growth of mice (10).
In addition to choosing gelatinized maca, choose organic maca to avoid pesticides if possible.
Some Maca recommendations:
How much maca is okay to consume?
Start with 1 teaspoon daily, in tea, smoothie, soup, or yogurt. Consume maca within recommended serving sizes and do not exceed these daily serving recommendations.
The Bottom Line
- Maca has shown some positive effects in studies on women trying to conceive but is more beneficial for men’s fertility overall. Outside of pregnancy, maca can help boost energy and libido and support women in managing their symptoms in the postmenopausal period.
- It is generally not recommended to start any herbal supplement, including maca, while pregnant or breastfeeding and to discuss with your doctor or midwife if you do.
- Overall, the number of studies done and the number of women in the studies are so few that more research needs to be done before it’s safe to say that maca is something that can be incorporated into your and your growing baby’s diet.
- Avoid maca if you have or have had hormone imbalances and conditions related to estrogen in the past or present, such as endometriosis or breast cancer, or if these run in your family. It may also be best to avoid maca if you have a thyroid condition.
- If you are not pregnant and would like to include maca, buy organic, gelatinized maca to reduce the risk of mold and increase nutrient absorption.
Written by: Alessandra D’Orazio, MS, RDN
Reviewed/edited by: Ryann Kipping, MPH, RDN, LDN, and Claire Gilmore, MSCN, CNS, LDN
High Blood Pressure/ Preeclampsia
Spirulina

Spirulina is a supplement that has been around for a long time. You may recall its popularity from the mid-2000s when it seemed everyone was taking it.
There are many purported health benefits, but is spirulina during pregnancy safe? Could it even provide benefits for pregnant women? Let’s take a look.
What is spirulina?
Spirulina comes from blue-green algae, or cyanobacteria, that grows in fresh and saltwater (1).
It’s an extremely popular supplement that’s recognized worldwide as the “ultimate superfood.” Spirulina is reported to increase energy, improve your mood, have potent antioxidants, and potentially help prevent heart disease, non-alcoholic fatty liver disease, and cancer (2, 3, 4).
Spirulina consumption dates back to the Aztecs in the 1400s and 1500s but is said to be more than 3.5 billion years old. The Aztecs would harvest spirulina, dry it, then mix it with other foods they ate (5).
The legend is that emperor Montezuma liked to eat fish and would send his followers hundreds of kilometers away from home to the ocean to catch the fish the emperor liked. And, spirulina was the food that kept them energized for the long haul.
Is spirulina safe during pregnancy?
There is not a lot of research done with spirulina investigating the effects it has on pregnant women, but there are a few articles that touch on the benefits and the risks that we will discuss throughout this article.
Studies in mice are promising, as they tend to show positive effects of spirulina during pregnancy.
In 2012, a study was published that demonstrated protective effects that spirulina’s antioxidants had on a certain type of neural tube defect that can occur in pregnant humans and mice (6).
Another study done in sub-Saharan African women who were pregnant saw an improvement in anemia status when they consumed spirulina in the third trimester of their pregnancies (7).
They actually found that taking spirulina was more effective than taking an iron and folic acid supplement. It was also noted that no adverse side effects were seen when the women took 1500 mg/day of spirulina in tablet form.
In a separate study with rats in 1998, the investigators found a higher iron storage level than that of the control group (8).
The evidence that is available is promising, but most of the studies have been done in mice, with few being completed in humans, especially pregnant women.
Of the studies that were promising, it seems that spirulina was mostly given or taken during the third trimester of pregnancy, which produces the least severe potential birth defects.

Nutrient breakdown
6 tablets, each 500 mg of spirulina
- Energy: 10 kcal
- Protein: 2 g
- Calcium: 20 mg
- Iron: 1.8 mg
- Sodium: 40 mg
- Vitamin B12: 3.6 ug
- Vitamin A: 7000 IU
All data provided by the USDA nutrient database.
Benefits of spirulina during pregnancy
Antioxidants & anti-inflammatory properties
The main component of spirulina is phycocyanin, which also gives spirulina its blue-green color. Phycocyanin is an antioxidant that helps fight free-radicals and inhibits inflammation.
Other researchers suggest spirulina can protect against oxidative stress and boost our immune system to help prevent many chronic health conditions (9, 4).
Iron
Phycocyanin also contributes to red blood cell production, which makes it popular among research studies to investigate the effects of spirulina (and phycocyanins) on the capabilities of algae during pregnancy and iron level changes.
Your body uses iron to make hemoglobin, which carries oxygenated cells throughout your body. When you are pregnant, you need more iron to accommodate your growing baby, and your growing body (10).
If you do not consume enough iron, then you could be at risk for developing iron-deficiency anemia.
When you have iron-deficiency anemia, you may notice you are fatigued and feel weaker than usual. You may also experience cold hands and feet and pale skin. Severe anemia has the potential to cause premature birth, low birth weight, and postpartum depression (10).
Iron can be found in meat, like chicken and beef, and can also be found in plants, such as cooked spinach and collard greens.
Protein
Two tablespoons of spirulina powder have 6 grams of protein, according to the USDA nutrient database (11).
Protein is vital to consume while you are pregnant. Protein helps your baby grow, especially his or her brain. It also plays a role in expanding your blood supply and growing your breast and uterine tissue.
Protein can be found in plant and animal-based foods, such as fish, chicken and other meats, nuts, peas, and beans.
As a plant-based protein, spirulina can contribute to protein and iron needs for those following a vegetarian diet during pregnancy.
Are there risks to consuming spirulina during pregnancy?
Oligohydramnios
In Malaysia, researchers found an association between women who took spirulina during pregnancy and a lower than normal amniotic fluid volume for gestational age, called oligohydramnios (12).
Amniotic fluid is vital for your baby’s development and can cause birth defects, low birth weight, and miscarriage (13).
Toxin exposure
While spirulina is not likely to harm you, it should be noted that sometimes microcystins can infiltrate this superfood as well as some heavy metals (2, 14).
However, it will make you feel better knowing a study completed in 2013 tested 25 different spirulina products and found that all 25 were within safe limits of toxic load. The most plentiful metals were Zinc and Nickel which are substantially less toxic than other metals like lead and arsenic (14).
Microcystins, on the other hand, cannot be broken down once ingested and can cause serious liver damage (15). A separate study in Montreal in 2016 tested cyanotoxin content of 18 brands and found that 8 contained some level of cyanotoxins, 4 were contaminated with microcystins, specifically (2).
In agreement with the researchers, product quality assurance is important. Find a high-quality product that is third-party tested for purity and potentially organic.
How to include spirulina in your diet
With the potential benefits of spirulina being increased iron levels and an extra punch of protein, you may be interested in taking it as a supplement, which is available as a tablet or powder.
The most popular way to add it to your diet is perhaps in your favorite smoothie, but you can also mix a spoonful into your water and drink it as is.
The Bottom Line
- Since the evidence is scant regarding the potential benefits and detriments of consuming spirulina while pregnant, it is best to speak with your doctor or dietitian regarding the safety of its consumption with your unique situation.
- With its promising effects on iron levels, spirulina may be a beneficial choice if you are experiencing anemia. It may also be a good addition to your diet if you are vegetarian.
- Again, be sure to discuss adding spirulina to your diet during pregnancy with your doctor or dietitian to be sure it is safe for you and your growing baby, especially if you are planning to forgo the iron capsule.
- As researchers P B Persson and A Zakrisson say it, spirulina may be an easy, cheap protein source, but people are stretching the truth by labeling it a “superfood” (16).
- Buy spirulina from a reputable brand, or store, that participates in third-party testing. This is the best way to ensure you are receiving a high-quality product that is free of any harmful toxins.
Athlete
Bed Rest
Turmeric
MTHFR Gene Mutation
Prenatal Vitamins
Multiple pregnancy
Protein Powders
Meal Plans
Gestational Diabetes
Green Tea
Celery Juice
This crazy green juice is all the rage right now which means many women are wondering if drinking celery juice during pregnancy is safe. Stores are sold out of celery and home juicing machines are flying off the shelf, but is this a trend you want to indulge in for you and your baby? We are outlining all the details below!
What is it?
While there is nothing new or revolutionary about juicing, it has returned to the spotlight after a popular book and a few popular “medical public figures” have touted it as a miracle juice.
It has taken the world by storm on Instagram as the newest selfie sidekick paired perfectly with a metal straw.
The idea is to juice 3 or more stalks of celery and consume it first thing in the morning before you eat anything else.
Although there isn’t much research backing it, people report changes in their bowel movements, skin, as well as other internal benefits, after starting this daily habit.
Is celery juice safe during pregnancy?
There is no research suggesting celery juice causes harm during pregnancy, but there is also no research suggesting specific benefits during pregnancy.
Many pregnant women are told juicing while pregnant is not safe because most fresh juices are not pasteurized. Pasteurization is a heat-treating process that reduces the chance of bacteria growth (1).
If you juice celery at home, it will not be pasteurized. If you do decide to consume home-juiced celery during pregnancy, ensure the celery has been carefully washed prior to juicing it.
Eating whole celery during pregnancy is perfectly safe. Increasing your vegetable intake can help increase micronutrients, prevent constipation, and also plays a role in fetal and infant growth (2).
Eating whole celery versus drinking it is different nutritionally.
Juicing celery requires much more celery than you could eat raw in one sitting with your favorite veggie dip.
A 16-ounce glass of celery juice usually contains around 9 stalks of celery, although you can use less to sip a little green juice.
Due to using a much larger quantity of celery in juice creation, the nutrients you obtain are higher which is appealing to women trying to up their nutrient intake during pregnancy.
Nutrient breakdown; whole celery versus celery juice:
In one large stalk of celery:
- Calories: 9 calories
- Carbohydrates: 1 g
- Sugar: 0.9 g
- Fat: 0 g
- Protein: 0.4 g
- Fiber: 1 g
- Potassium: 166 mg
- Calcium: 25.6 mg
- Sodium: 51 mg
In an 8 oz. glass of celery juice:
About 3-4 large stalks
- Calories: 42 calories
- Carbohydrates: 9 g
- Sugar: 6 g
- Fat: 0 g
- Protein: 2 g
- Fiber: 4 g (with pulp, so if you blend it, not juice it)
- Potassium: 670 mg
- Calcium: 100 mg
- Sodium: 215 mg
All values provided by the USDA nutrient database.
Are there benefits to consuming celery juice during pregnancy?
Celery, raw or juiced, is mainly composed of water, hence it can help keep you hydrated.
It is important to increase fluid intake as your pregnancy progresses because body weight and blood volume are changing rapidly.
People who drink celery juice regularly report increased or better-regulated bowel movements, although not everyone will receive these benefits.
Again, you are likely to see this benefit also from eating whole celery due to the fiber content.
This can be beneficial to pregnant women because a common symptom of pregnancy and taking some prenatal vitamins is constipation.
One study in rats suggests celery seed helps lower blood pressure (3). A study in China showed celery juice specifically reduced blood pressure in 14 of 16 patients (4).
There are no studies showing celery juice affects blood pressure in pregnancy specifically.
 Are there potential side effects?
Are there potential side effects?
As stated above, there is no research suggesting celery juice is harmful in pregnancy, however, there are no specific benefits to consuming celery juice during pregnancy.
Drinking the juice of any fruit or vegetable typically means you will be ingesting more sugar. While this is sugar naturally found in the produce, it still contributes to the rise in your blood sugar.
Secondly, the fiber content is lost when you juice celery.
The fiber in foods helps to keep us full and helps regulate our bowel movements. This is important during pregnancy due to the increased chance of constipation.
Dismissing the fiber in this vegetable would not be utilizing it in its best form. To keep some of the fiber, blend the celery as opposed to juicing it.
 The Bottom Line
The Bottom Line
- Celery and celery juice are generally safe during pregnancy. Remember to wash all produce thoroughly before consuming it.
- While it is recommended that you do not start anything new during pregnancy, increasing your vegetable intake has many benefits and celery juice can contribute to your overall fluid intake.
- If you enjoyed celery juice prior to becoming pregnant, and still find it appealing when pregnant, it is fine to continue including it in your diet.
By Lauren Gannon, RDN, and Ryann Kipping, RDN, CLEC | Owner & Founder
Almond Milk
Non-dairy “milks” are the latest health trend to hit all major grocery stores and your favorite coffee shops, but what about almond milk during pregnancy?
Is adding almond milk to your smoothie the best option for your body and your baby?
Many people make the switch from dairy milk to almond milk because of dietary or allergy concerns, but some who continue to drink dairy milk may just want to add variety to their diet or enjoy it because of the taste or consistency.
Regardless of the reason you drink almond milk, we are covering everything you need to know here.
Is almond milk safe during pregnancy?
There is no research on almond milk during pregnancy as it is still a relatively new product on the market.
Almonds themselves are safe and quite a nutritious option for pregnancy due to their healthy fats, vitamin E and fiber content, but what happens when we turn them into liquid?
To make almond milk, you simply need almonds and water which lends to believe it is safe during pregnancy. However, not all almond milks are created equal.
For consistency, added flavor, and extended shelf-life many beverage companies put various preservatives or food additives in their almond milks. Some of these are completely harmless, but others have shown potentially negative effects.
One particular food additive, carrageenan, is used to thicken, emulsify, and extend the shelf-life of certain products. It is often found in vegan or vegetarian products since it is derived from plants.
A few studies have found a possible link to increased inflammation and gastrointestinal issues with excessive consumption of carrageenan and so, the National Organic Standards Board removed it from the list of approved ingredients (1, 2).
There may also be other “gums” which are used for the same reasons as carrageenan but provide no nutritional value.
At the end of this article, we will discuss what to look for when purchasing almond milk at the store.
Is almond milk good for pregnancy?
As previously stated, there is no research on drinking almond milk during pregnancy.
While almond milk can certainly fit into a healthy prenatal diet, it is important to note cow’s milk and almond milk are nutritionally not the same. In fact, most non-dairy milks do not share the same nutrition properties as cow’s milk (3).
Some almond milks are fortified with nutrients such as vitamin D, vitamin B12, and calcium making it a good choice for those who are allergic or sensitive to cow’s milk.
Fortified or not, almond milk is not a source of protein, iodine, or selenium so ensure you are getting plenty of these three nutrients elsewhere.
Almond milk contains fewer calories, less sugar (if unsweetened), less protein, and fewer nutrients than cow’s milk.
A “lower calorie” food can quickly become appealing, but pregnancy is generally not a time when we want to “count calories” or intentionally choose “low-calorie” foods.
And, although cow’s milk does technically contain more sugar and therefore, more carbohydrates, this is naturally occurring.
Overall, almond milk can fit into a healthy prenatal diet and an unsweetened, potentially fortified option could be perfect for those with a dairy allergy or sensitivity.
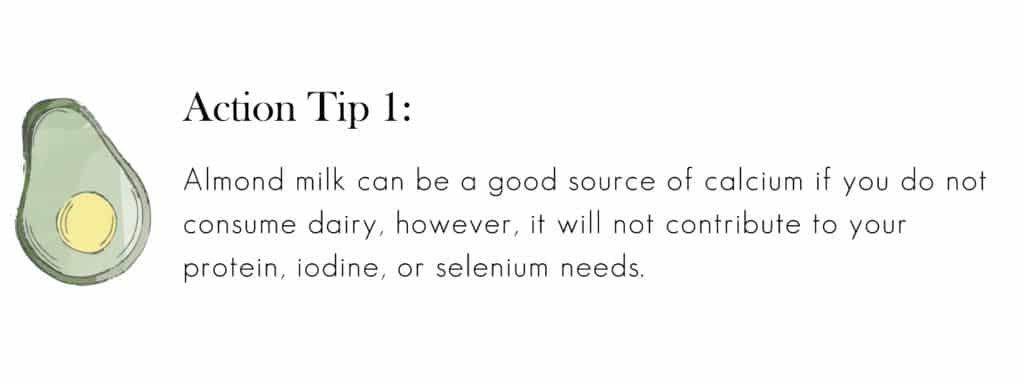
Almond milk vs. cow’s milk nutrient breakdown
Replacing all your dairy milk with almond milk is not a direct swap as you can see.
Below are the nutritional values of both dairy milk and almond milk for an 8 oz. or 1 cup serving.
Almond milk, unsweetened, unfortified (4)
- Calories: 37
- Fat: 3 g
- Protein: 1 g
- Carbs: 1 g
- Fiber: < 1 g
- Sugar: < 1 g
- Calcium: 481 mg
- Vitamin D: 0 g
- Vitamin B12: 0 g
- Potassium: 163 mg
- Choline: 0 mg
Whole cow’s milk (5)
- Calories: 149
- Fat: 8 g
- Protein: 8 g
- Carbs: 12 g
- Fiber: 0 g
- Sugar: 12 g
- Calcium: 276 mg
- Vitamin D: 127 IU
- Vitamin B12: 1.1 mcg
- Potassium: 322 mg
- Choline: 35 mg
Dairy from cows naturally provides many nutrients important for pregnancy such as protein, calcium, iodine, vitamin B12, probiotics, and more, so if you aren’t allergic, it is beneficial for you and for the baby during pregnancy.
What about other non-dairy milks during pregnancy?
Soy milk is a popular non-dairy beverage that has been around for ages, but more recently we have seen practically everything be liquified.
Other non-dairy “milks” include:
- Oat milk
- Cashew milk
- Rice milk
- Coconut milk
- Pea milk
- Hemp seed milk
- Flaxseed milk
All of the above are safe to consume during pregnancy, but again contain a wide variety of nutrients likely not equivalent to cow’s milk. Like anything else, moderation is key.
Tips for purchasing almond milk
As stated above, all kinds of milk are not created equal nor are all kinds of almond milk. Below are some things to consider when reviewing almond milk options during your next grocery trip.
- Choose unsweetened varieties to limit added sugar intake
- Choose an organic option, if you can
- Find one with two simple ingredients: almonds and water
- Or, pick one without carrageenan
- If you’re worried about nutrient intake, choose one that’s fortified
Alternatively, you can always make your own almond milk!
There are a number of recipes floating around the internet touting it’s easy and has a delicious flavor.
The Bottom Line
- There is currently no research on almond milk during pregnancy, but due to the nature of the product it is safe to consume in moderation.
- Since almond milk is not equivalent to cow’s milk in the way of nutrients, it is important that you make sure you are getting these nutrients elsewhere in your diet.
- When purchasing almond milk during pregnancy, make sure to avoid added sugars and unnecessary additives such as carrageenan.
By Lauren Gannon, RDN, and Ryann Kipping, RDN, CLEC | Owner & Founder
Juicing
Juicing has gained a lot of popularity in recent years. You may even have a friend or two who’ve done a juice cleanse, and maybe you have too. Now that you’re pregnant, you may be wondering: is juicing during pregnancy safe for me and my baby?
What is juicing?
Juicing involves squeezing (literally) the nutrients out of a fruit or vegetables, or both. The process eliminates all solid matter that was part of the fruit or vegetable. There are many reasons why an individual would juice, with a popular one being to “detox”.
When someone goes on a juice cleanse to detox, it can last anywhere from 3 days to several weeks.
The belief is that the nutrients in the juice will eliminate built-up toxins in the body either by resting your organs, stimulating your liver, improving circulation, or passing them through urine or bowel movements (1).
Is juicing safe during pregnancy?
When you juice, you are eliminating an incredibly important nutrient from your diet, fiber.
During pregnancy, a lot of hormonal changes are happening, and oftentimes that can lead to constipation. Fiber is a great way to get everything moving again, and eliminating it from such a stellar food source is not recommended.
Fiber also lowers your risk for several diseases.
It does this by helping to sweep cholesterol away and out of the body when you have a bowel movement, and by lessening the blood glucose response by your body, which in turn keeps insulin levels lower too (1).
Choosing to participate in a juice cleanse while pregnant is not a good idea.
Your body needs adequate nutrition to fuel your baby’s growth, and doing a juice cleanse will not give you the number of calories or protein that you need to help your baby grow.
Below is the fiber difference between eating an apple versus drinking the juice.
Apple, whole
Fiber: 4.37 g
Apple, juiced
Fiber 0.2 g
All nutrients obtained from the USDA nutrient database.
It’s also important to note you often juice many more pieces of fruit than you would normally eat in one sitting. This results in more sugar consumption. Yes, this is naturally occurring sugar, but it still contributes to the rise in your blood sugar.
For example, to make 8 ounces of orange juice, it takes 4-5 oranges. You could easily drink 1 cup of orange juice, but most of us wouldn’t eat 5 oranges in one sitting.
We will discuss blood sugar and gestational diabetes risk in more detail below.
Are there benefits to juicing during pregnancy?
If you’ve ever had a conversation with someone, or read a blog post by an individual who completed a juice cleanse, then you know they usually swear it works and that they feel better.
When you juice, recipes include whole, fresh fruit and vegetables, which is exactly what the dietitian ordered. It’s a convenient way to get in most, if not all, of your fruit and vegetable servings in a day, as well as vitamins, minerals, and antioxidants.
When you juice, you also tend to avoid processed foods, which is something many people are interested in. That means avoiding dietary sources of heavy metals, and other scary-sounding additives and by-products (2).
While these anecdotal stories are inspiring, and may even convince you to participate in a juice cleanse, there is no sound scientific evidence to support any of what juicing claims to do (3).
The liver, one of the largest organs in our body helps us naturally eliminate potential toxins (4).
Learn more about celery juice during pregnancy, specifically, in a separate note.
Learn more about celery juicing during pregnancy
What about morning sickness?
If you’re having morning sickness, and find it difficult to keep food down, then juicing may be a viable option to help you get some of the nutrients you need for the time being.
Additionally, consider smoothies which also allows you to get a lot of nutrients in one sitting, and can also include plenty of protein to help you reach your daily needs.
Are there downsides to juicing during pregnancy?
Food safety
If you would like to consume a juice every now and then (or one every day to supplement your intake), be sure you are buying pasteurized juices.
By using high heat, the pasteurization process reduces the chances of harmful bacteria contamination, which can hurt your unborn baby and cause permanent abnormalities (5).
If you are home juicing, you will obviously not have access to commercial kitchen equipment to pasteurize your juice. For this reason, it is very important you thoroughly wash all produce prior to juicing it, even fruits that you don’t eat the peel.
Additionally, if you want to be extra cautious, you can bring your juice to a boil for at least one minute prior to consuming it.
If you live in a more “health-conscious” town or a bigger city, there may be juice shops around every block. They may or may not heat treat their juices. Don’t be afraid to ask or inquire about their juicing process.
After making an assessment of their store, food quality, and food safety practices, use your best judgment to make the right decision for you.
High blood sugar
Before buying a juicer or getting a local juice co punch card, it’s important to make sure you are not at risk for gestational diabetes.
Since the fiber from the fruits and vegetables is juiced out, you have nothing left to aid in slowing down how fast your body absorbs the natural sugar, and you’re left with sugary nutrition water – which isn’t problematic for everyone.
To reinforce the importance of fiber, we need to discuss another role of this crucial nutrient. It helps to control the rise in our blood sugar making the sugar in whole fruits less of an issue.
Some studies have found a link between high fruit juice intake and increased risk of diabetes in and outside of pregnancy (6, 7).
Check with your doctor to ensure your blood sugar levels are within a normal range before you consume juices regularly.
The Bottom Line
While juicing can be fun, and create community if you involve your friends, you may want to re-think your juicing decisions, at least until after your baby is born.
Enjoying a pasteurized juice, or a homemade one with adequately washed produce, once in a while will not harm you or your baby, and can give you a vitamin boost.
Check with your doctor or dietitian if you plan to incorporate juices regularly into your prenatal diet.
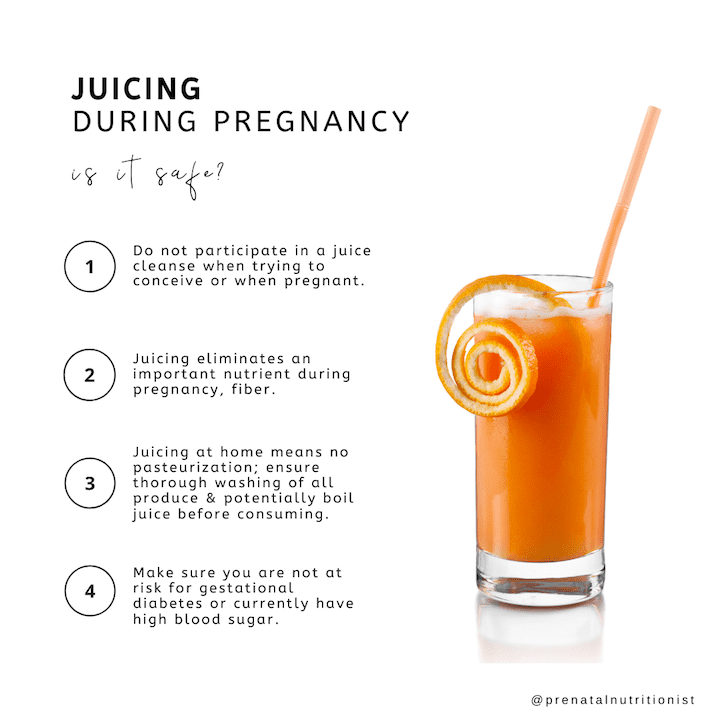
If you would like to keep the fiber content of your delicious drink high, then consider making a smoothie instead. You still get all of the amazing nutrients that fruit and vegetables have to offer, while not sacrificing the fiber content, and the rest of the solid material.
By Alexa D’ Orazio, MS, RDN and Ryann Kipping, MPH, RDN, CLEC | Owner & Founder